Back
CPPS Pelvic Floor Therapy: Understanding, Benefits, and Process
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 10/20/2023

Overview
Definition of CPPS
CPPS, or chronic pelvic pain syndrome, is a condition characterized by persistent pain in the pelvic region. It is a common condition that affects both men and women, and can have a significant impact on quality of life.
Explanation of Pelvic Floor Therapy
Pelvic floor therapy is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues in the pelvic floor. It involves a variety of exercises and techniques to help improve strength, flexibility, and coordination in this area.
Importance of Pelvic Floor Therapy for CPPS Treatment
Pelvic floor therapy is an essential component of CPPS treatment. The pelvic floor muscles play a crucial role in supporting the pelvic organs and maintaining bladder and bowel control. When these muscles are weak or dysfunctional, it can contribute to CPPS symptoms. Pelvic floor therapy can help alleviate pain and improve overall pelvic floor function, leading to better management of CPPS.
By addressing the root cause of CPPS, pelvic floor therapy can also help reduce the need for pain medication and other invasive treatments. It is a safe and effective approach that can provide long-term relief for those suffering from CPPS.
Brief Overview of the Following Sections
In the following sections, we will delve deeper into the specifics of pelvic floor therapy for CPPS. We will discuss the different techniques and exercises used in this form of therapy, as well as the benefits and potential side effects. Additionally, we will explore the role of pelvic floor therapy in a comprehensive treatment plan for CPPS, and provide tips for finding a qualified pelvic floor therapist.
Understanding CPPS
Definition and Symptoms of CPPS
CPPS stands for Chronic Pelvic Pain Syndrome, which is a condition that causes persistent pain in the pelvic region. It is also known as chronic prostatitis, as it primarily affects men, but can also occur in women. The main symptom of CPPS is pain in the pelvic area, which can range from mild discomfort to severe and debilitating pain. Other symptoms may include urinary problems, sexual dysfunction, and psychological distress.
Causes of CPPS
The exact cause of CPPS is unknown, but it is believed to be a combination of physical, psychological, and neurological factors. Some possible causes include inflammation of the prostate or pelvic muscles, nerve damage, and psychological stress. In some cases, there may be no identifiable cause, making treatment more challenging.
Prevalence and Risk Factors
CPPS is a common condition, affecting approximately 10-15% of men worldwide. It is more prevalent in men over the age of 50 and those with a history of urinary tract infections or prostate issues. Other risk factors may include a sedentary lifestyle, high levels of stress, and certain medical conditions such as irritable bowel syndrome or fibromyalgia.
Impact on Quality of Life
CPPS can have a significant impact on a person's quality of life, both physically and emotionally. The chronic pain and discomfort can make it challenging to perform daily activities and can lead to feelings of frustration, anxiety, and depression. It can also affect relationships and sexual function, causing further distress. Seeking treatment for CPPS is essential to improve overall well-being and quality of life.
Pelvic Floor Anatomy and Function
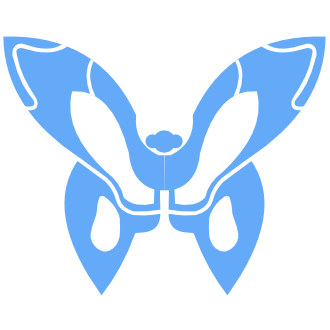
Explanation of Pelvic Floor Muscles
The pelvic floor muscles are a group of muscles that form a sling-like structure at the bottom of the pelvis. They are responsible for supporting the pelvic organs, including the bladder, uterus, and rectum. These muscles are also involved in controlling urinary and bowel function, as well as sexual function.
Role of Pelvic Floor Muscles in Urinary and Sexual Function
The pelvic floor muscles play a crucial role in urinary and sexual function. They help to control the flow of urine and stool, and also contribute to sexual sensation and orgasm. In women, these muscles are also involved in childbirth and can help to prevent urinary incontinence and pelvic organ prolapse.
How Pelvic Floor Dysfunction Can Contribute to CPPS
CPPS, or chronic pelvic pain syndrome, is a condition characterized by chronic pain in the pelvic region. Pelvic floor dysfunction, which can include tightness, weakness, or spasms in the pelvic floor muscles, is a common contributing factor to CPPS. When these muscles are not functioning properly, it can lead to pain, discomfort, and other symptoms in the pelvic area.
Importance of Pelvic Floor Muscle Relaxation and Coordination
In order to effectively treat CPPS, it is important to address any issues with pelvic floor muscle relaxation and coordination. This may involve exercises to strengthen and relax the muscles, as well as techniques such as biofeedback and pelvic floor physical therapy. By improving the function of the pelvic floor muscles, symptoms of CPPS can be reduced or eliminated.
Benefits of Pelvic Floor Therapy for CPPS
Relieving Pelvic Pain and Discomfort
Pelvic floor therapy is a non-invasive treatment option for chronic pelvic pain syndrome (CPPS) that focuses on the muscles, ligaments, and connective tissues in the pelvic region. By targeting these specific areas, pelvic floor therapy can help to alleviate pain and discomfort caused by CPPS. This can be especially beneficial for individuals who have tried other treatments without success, as pelvic floor therapy addresses the root cause of the pain rather than just managing symptoms.
Improving Urinary and Sexual Function
The pelvic floor muscles play a crucial role in urinary and sexual function. When these muscles are tight or weak, it can lead to issues such as urinary incontinence, frequent urination, and sexual dysfunction. Pelvic floor therapy can help to strengthen and relax these muscles, improving bladder control and sexual function. This can greatly improve the quality of life for individuals with CPPS, as these issues can be embarrassing and affect daily activities.
Reducing Muscle Tension and Spasms
CPPS can cause the pelvic floor muscles to become tense and spasm, leading to pain and discomfort. Pelvic floor therapy uses techniques such as manual therapy, stretching, and relaxation exercises to release tension and reduce spasms in these muscles. This can provide significant relief for individuals with CPPS, as well as prevent future flare-ups.
Enhancing Overall Quality of Life
Chronic pelvic pain can greatly impact an individual's quality of life, affecting their physical, emotional, and social well-being. By addressing the underlying issues causing CPPS, pelvic floor therapy can help to improve overall quality of life. This can include reducing pain and discomfort, improving bladder and sexual function, and increasing mobility and flexibility. Additionally, pelvic floor therapy can also help to reduce stress and anxiety associated with CPPS, leading to a better overall sense of well-being.
Types of Pelvic Floor Therapy
Manual Therapy Techniques
Manual therapy techniques involve the use of hands-on techniques to address muscle tension and dysfunction in the pelvic floor. These techniques are typically performed by a trained physical therapist and can provide relief from pelvic pain and other symptoms.
Some common manual therapy techniques used in pelvic floor therapy include:
Internal Trigger Point Release:
This technique involves applying pressure to specific trigger points in the pelvic floor muscles to release tension and improve blood flow.Myofascial Release:
This technique involves gentle stretching and massage of the connective tissue surrounding the pelvic floor muscles to improve mobility and reduce pain.Soft Tissue Mobilization:
This technique involves using gentle pressure and stretching to release tension in the muscles and soft tissues of the pelvic floor.
Biofeedback Therapy
Biofeedback therapy is a non-invasive technique that uses sensors to measure muscle activity and provide visual or auditory feedback to the patient. This can help patients learn how to control and relax their pelvic floor muscles, which can be beneficial for conditions such as urinary incontinence and pelvic pain.
During a biofeedback session, the therapist will place sensors on the pelvic floor muscles and the patient will perform exercises while watching the feedback on a screen or listening to audio cues. This can help the patient learn how to properly engage and relax their pelvic floor muscles.
Pelvic Floor Exercises
Pelvic floor exercises, also known as Kegel exercises, are a key component of pelvic floor therapy. These exercises involve contracting and relaxing the pelvic floor muscles to improve strength, control, and coordination.
In addition to Kegel exercises, pelvic floor therapy may also include stretching and strengthening exercises for other muscles that support the pelvic floor, such as the hips and core muscles.
Relaxation Techniques
Relaxation techniques can be helpful for patients with pelvic floor muscle tension and pain. These techniques can help reduce stress and tension in the body, which can contribute to pelvic floor dysfunction.
Some common relaxation techniques used in pelvic floor therapy include:
Deep Breathing:
Deep breathing exercises can help relax the pelvic floor muscles and promote relaxation throughout the body.Meditation and Mindfulness:
These techniques can help patients become more aware of their body and learn to release tension and stress in the pelvic floor muscles.
Pelvic Floor Therapy Process
Initial Assessment and Evaluation
The first step in pelvic floor therapy is an initial assessment and evaluation. This typically involves a thorough review of the patient's medical history and symptoms. The therapist will also perform a pelvic floor muscle examination to assess the strength, tone, and coordination of the muscles. This information will help the therapist understand the root cause of the patient's symptoms and develop an appropriate treatment plan.
Individualized Treatment Plan
Based on the assessment, the therapist will create an individualized treatment plan for the patient. This plan may include a combination of techniques such as pelvic floor exercises, manual therapy, biofeedback, and relaxation techniques. The therapist will also determine the frequency and duration of therapy sessions based on the severity of the patient's symptoms and their progress.
Progress Tracking and Adjustments
As the patient progresses through therapy, the therapist will monitor their symptoms and track their improvements. If necessary, the treatment plan may be adjusted to better suit the patient's needs. This could include modifying the types of techniques used or changing the frequency and duration of therapy sessions. Regular check-ins with the therapist will ensure that the treatment plan is effective and making progress towards the established goals.
Maintenance and Long-Term Management
Pelvic floor therapy is not a one-time fix, and it is essential for patients to continue exercises and techniques at home to maintain their progress. The therapist will provide guidance on how to continue these exercises and techniques independently. Follow-up appointments may also be scheduled to monitor the patient's progress and make any necessary adjustments to their long-term management plan.
If you are experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment