Back
How Does Dry Needling Help Pelvic Floor Patients with Low Back Pain and Pelvic Floor Dysfunction?
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 9/20/2023

We now offer dry needling treatment!
Dry needling is a technique used by physical therapists and other trained professionals such as acupuncturists to treat musculoskeletal pain and dysfunction by using a thin monofilament needle to penetrate the skin to address any underlying muscular trigger points. It is a western medicine technique in which needles are inserted to release tension, knots, and pressure points in muscle.
Dry needling can address:
Low back / Joint pain
Pelvic pain
C-section scar tissue
Overuse Injuries
Night cramps
Sacral pain
Tailbone pain
Pelvic Floor Dysfunctions
Phantom pain
Here at Pelvic Health, we commonly treat conditions related to low back pain and the pelvic floor. According to a 2021 study, dry needling can treat irregular periods (dysmenorrhea), urinary incontinence, and chronic pelvic pain.
There is moderate relief and improved symptoms when initiating dry needling 1 week prior to onset of menstruation. Since referred pain is well documented for the uterus and because the uterus shares common pain fiber pathways with the abdominal muscles, needling procedures directed to the abdomen can limit the pain response to the uterus, thereby decreasing the severity of pain associated with primary dysmenorrhea. Given that high levels of pain chemicals (prostaglandins) may activate latent trigger points in abdominal muscles, trigger point dry needling may be a useful technique in women with dysmenorrhea.
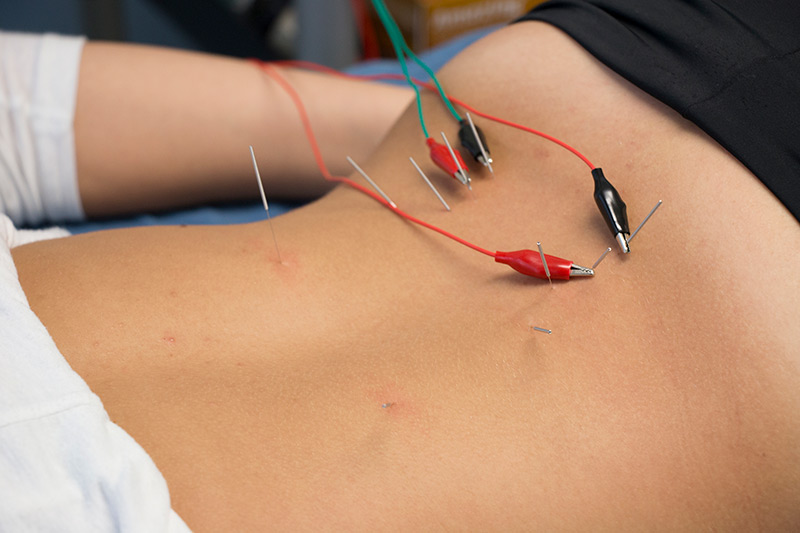
For urinary incontinence, there are many high quality trials that support the use of electroacupuncture, in which a small electric current is passed between pairs of the monofilament needles (see photo below). According to a 2017 study, after 6 weeks of electroacupuncture (3 times per week), patients with stress incontinence reported significantly less urine leakage, reduced frequency of incontinence episodes, improved function (International Consultation on Incontinence Questionnaire-Short Form) and satisfaction following treatment.
As for chronic pelvic pain, the pain may be stemming from conditions like interstitial cystitis, irritable bowel syndrome, or chronic vulvodynia. In these chronic cases of vulvodynia in particular, patients reported 50% less pain after the first session and 100% pain relief after the 2nd session. This reduction in pain was also maintained in the 9 month follow up examination. dry needling for abdominal, hip and pelvic floor muscles with trigger points may be useful in patients with pelvic floor dysfunction.
How exactly does dry needling work? The idea behind the needle is to penetrate the skin and clear out excessive acetylcholine (a neurotransmitter that activates muscle) from the neuromuscular junction, and this will interrupt the cycle of hypertonicity (tightness) in the trigger point, thereby resolving the issue.
Do you think you will benefit from this modality?
Please reach out to us here at the Pelvic Health Center in Madison, NJ to set up an evaluation & assessment! Feel free to call us 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Works Cited:
Fellowship, A. A. M. T., Paula F Prestemon PT on April 24, & PT, P. F. P. (2017, April 15). Management of pelvic floor dysfunction: Dry needling, exercise & electroacupuncture. OSTEOPRACTIC. Retrieved June 7, 2022
Fellowship, A. A. M. T. (2021, May 15). Spinal manipulation and acupuncture in women with primary dysmenorrhea: Clinical Utility & Evidence Summary. OSTEOPRACTIC. Retrieved June 7, 2022
Read More:
Exercise to reduce pelvic floor dysfunction associated with childbirth?? By Amalie Malka Flamm on 7/25/2024 What exercises can help reduce pelvic floor dysfunction associated with childbirth? Why does my taint hurt (male)? By Shannon Strauch, PTA, STMT-1 on 7/24/2024 Where is your perineum, what is it's function, and why do you have pain?
Are you ready to live pain free?
Request An Appointment