Back
Ehlers Danlos Syndrome and Pelvic Complications
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 9/20/2023
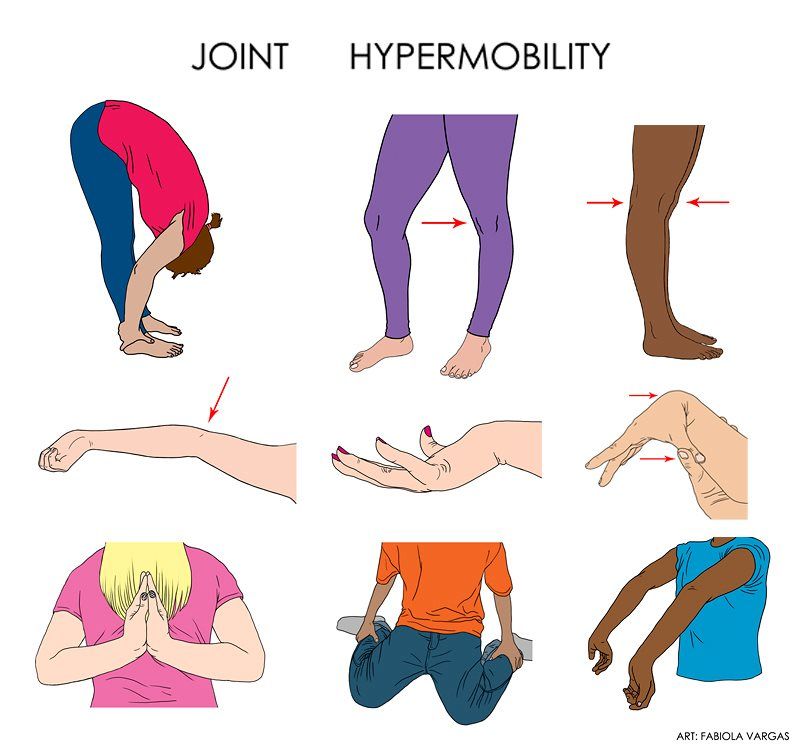
Ehlers Danlos Syndrome (EDS) is a connective disorder disorder that causes excessive mobility (hypermobility) in one’s joints. Connective tissue properties include collagen and elastin, and EDS is categorized as defective collagen production. When linking EDS and pelvic conditions, it should be noted that collagen rich areas include the bladder, uterus, and pelvic floor ligaments . Symptoms of EDS can involve chronic pain, fatigue, prolonged wound healing, and a host of musculoskeletal/ pelvic dysfunctions.
EDS can be diagnosed using outcome measures such as Beighton, Brighton, and Villefranche. Other methods were physical exam without specific criteria, patient self-report, genetic testing, and skin biopsies. This condition is prevalent among females, and we will dive into the urinary and gynecological involvement of this syndrome.
Women with EDS report urinary issues including stress incontinence, urge incontinence, pain with intercourse, and nocturnal urinary incontinence, recurrent urinary tract infections (UTIs), bladder outlet obstruction, bladder pain, blood in urine, urinary retention, and voiding dysfunction.EDS causes pelvic laxity and instability, and will warrant a thorough musculoskeletal and possibly internal exam to address any weakness, incoordination, or neuromuscular deficit that can be attributing to the urinary dysfunction.
Gynecologically, women with EDS are more prone to report pelvic organ prolapse (POP), menstrual complications including irregular menses, intermenstrual bleeding; polycystic ovary syndrome (PCOS), endometriosis, endometrial cysts, uterine fibromas, pelvic or vulva varicose veins; and pelvic floor dysfunctions.
After pregnancy, those with EDS in particular are more susceptible to pelvic organ prolapse. Prolapse is the downward distension of the uterus, intestine, rectum, or bladder from its normal position. The supportive, collagenous fibers of the pelvic floor are compromised, causing organs to descend through the vaginal cavity.
A multimodal approach is needed to address the different facets of this disorder, and pelvic physical therapy is a great conservative, non pharmacological approach to building strength, learning activity modifications, and managing symptoms for all genders.
Exercises can include controlled and eccentric stretches, isometrics, core stabilization, and more. Activity modifications can include lifting biomechanics, ergonomics, and an environmental/task analysis to optimize work or school. Symptom management can include pelvic floor elevation and external tools to modulate organ descent.
Please reach out to us here at the Pelvic Health Physical Therapy Center in Madison, NJ to set up an evaluation & assessment! Feel free to call us 908-443-9880 or email us at contact@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment