Back
Exercises for Gastroparesis: Pelvic Physical Therapy Guide
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 10/19/2023
Exercises for Gastroparesis Pelvic Physical Therapy
Overview
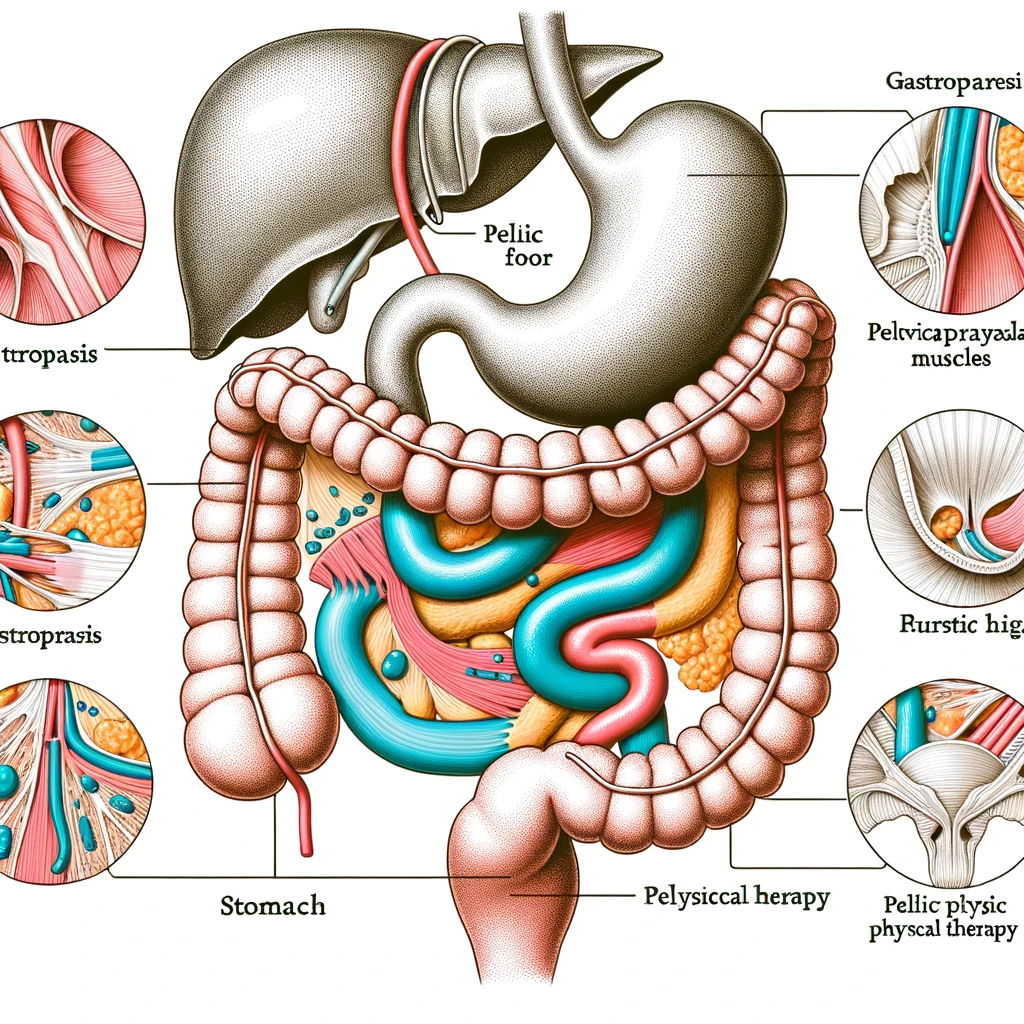
Gastroparesis is a condition in which the stomach muscles do not function properly, causing delayed emptying of food into the small intestine. This can lead to symptoms such as nausea, vomiting, bloating, and abdominal pain. Pelvic physical therapy is a non-invasive treatment option that focuses on the muscles and structures of the pelvic floor to improve symptoms of gastroparesis.
Definition of Gastroparesis
Gastroparesis is a chronic condition that affects the stomach muscles, causing them to work slowly or not at all. This can be caused by damage to the vagus nerve, which controls the movement of food through the digestive tract, or by other underlying health conditions such as diabetes or autoimmune disorders. Symptoms of gastroparesis can range from mild to severe and can significantly impact a person's quality of life.
Role of Pelvic Physical Therapy in Managing Gastroparesis
Pelvic physical therapy is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues of the pelvic floor. These muscles play a crucial role in digestion and can become tight or weak in individuals with gastroparesis. Pelvic physical therapy can help improve the function of these muscles, leading to better digestion and a reduction in symptoms.
Benefits of Exercises for Gastroparesis
Exercises for gastroparesis can help improve the strength and coordination of the pelvic floor muscles, which can aid in the movement of food through the digestive tract. These exercises can also help reduce tension and tightness in the pelvic floor, which can contribute to symptoms such as bloating and abdominal pain. Additionally, pelvic physical therapy can provide education on proper posture and breathing techniques to support digestion and improve overall pelvic health.
Understanding the Pelvic Floor
Anatomy of the Pelvic Floor
The pelvic floor is a group of muscles, ligaments, and connective tissue that form a sling-like structure at the bottom of the pelvis. It is made up of three layers: the superficial perineal layer, the deep urogenital diaphragm, and the pelvic diaphragm. These muscles work together to support the pelvic organs, including the bladder, uterus, and rectum.
Functions of the Pelvic Floor
The pelvic floor has several important functions, including maintaining continence, supporting the pelvic organs, and aiding in sexual function. It also plays a role in stabilizing the spine and pelvis during movement and providing structural support for the pelvic organs.
How Gastroparesis Affects the Pelvic Floor
Gastroparesis is a condition in which the stomach takes longer than normal to empty its contents into the small intestine. This can lead to a variety of symptoms, including bloating, nausea, and abdominal pain. These symptoms can also affect the pelvic floor, as the muscles may become tense or weakened due to the discomfort and inflammation caused by gastroparesis.
Importance of Pelvic Floor Muscle Strength in Managing Gastroparesis
Strengthening the pelvic floor muscles can be beneficial for individuals with gastroparesis. Strong pelvic floor muscles can help improve bowel and bladder function, reduce symptoms of pelvic pain, and support the pelvic organs. Additionally, pelvic physical therapy can help individuals with gastroparesis learn how to relax and release tension in the pelvic floor muscles, which can help alleviate symptoms and improve overall quality of life.
Consultation with a Healthcare Provider Before Starting Exercises
Before beginning any exercises for gastroparesis pelvic physical therapy, it is crucial to consult with a healthcare provider. They can assess your individual situation and determine if pelvic physical therapy is appropriate for you. They can also provide guidance on the types of exercises that may be most beneficial and any modifications that may be necessary based on your specific condition.
Additionally, your healthcare provider can monitor your progress and make any necessary adjustments to your treatment plan to ensure that you are getting the most out of your pelvic physical therapy.
Types of Exercises for Gastroparesis
Relaxation Exercises
Relaxation exercises can help to reduce stress and tension in the body, which can improve symptoms of gastroparesis. These exercises focus on deep breathing and muscle relaxation techniques.
Deep Breathing:
This exercise involves taking slow, deep breaths, filling the lungs completely and then exhaling slowly. This can help to relax the body and reduce stress.Diaphragmatic Breathing:
Also known as belly breathing, this exercise involves breathing deeply into the belly, expanding the diaphragm and filling the lungs. It can help to improve digestion and reduce bloating.Progressive Muscle Relaxation:
This exercise involves tensing and relaxing different muscle groups in the body, starting from the feet and working up to the head. It can help to release tension and promote relaxation.
Strengthening Exercises
Strengthening exercises can help to improve muscle tone and function in the pelvic area, which can improve symptoms of gastroparesis. These exercises focus on the pelvic floor muscles, which play a key role in digestion.
Pelvic Floor Muscle Contractions:
Also known as Kegel exercises, these involve contracting and relaxing the muscles of the pelvic floor. This can help to improve muscle strength and control.Bridge Pose:
This yoga pose involves lying on your back with your knees bent and lifting your hips off the ground. It can help to strengthen the pelvic floor muscles and improve digestion.Squats:
This exercise involves standing with your feet shoulder-width apart and squatting down as if you are sitting in a chair. It can help to strengthen the pelvic floor muscles and improve digestion.
Coordination Exercises
Coordination exercises can help to improve the coordination and control of the pelvic floor muscles, which can improve symptoms of gastroparesis. These exercises focus on the movement and positioning of the pelvis.
Pelvic Tilts:
This exercise involves tilting the pelvis forward and backward while standing or lying down. It can help to improve coordination and control of the pelvic floor muscles.Pelvic Clock:
This exercise involves imagining a clock on the floor and moving the pelvis to different numbers on the clock. It can help to improve coordination and control of the pelvic floor muscles.Pelvic Floor Drops:
This exercise involves relaxing and dropping the pelvic floor muscles while standing or sitting. It can help to improve coordination and control of the pelvic floor muscles.
Stretching Exercises
Stretching exercises can help to improve flexibility and range of motion in the pelvic area, which can improve symptoms of gastroparesis. These exercises focus on stretching the muscles in the hips, hamstrings, and glutes.
Hip Flexor Stretch:
This stretch involves kneeling on one knee and leaning forward, stretching the front of the hip. It can help to improve flexibility and reduce tension in the hip muscles.Hamstring Stretch:
This stretch involves sitting on the ground with one leg extended and leaning forward, stretching the back of the thigh. It can help to improve flexibility and reduce tension in the hamstring muscles.Glute Stretch:
This stretch involves lying on your back with one leg crossed over the other and pulling the knee towards the opposite shoulder. It can help to improve flexibility and reduce tension in the glute muscles.
How to Perform the Exercises
Proper Body Positioning
When performing exercises for gastroparesis pelvic physical therapy, it is important to maintain proper body positioning to ensure the effectiveness of the exercises and prevent injury. This includes sitting or standing with good posture, keeping the spine neutral, and engaging the core muscles. It may also be helpful to use props such as pillows or a stability ball to support the body during certain exercises.
Breathing Techniques
Breathing techniques are an important aspect of pelvic physical therapy exercises for gastroparesis. Proper breathing can help relax the pelvic floor muscles and improve blood flow to the area. It is recommended to inhale deeply through the nose and exhale slowly through the mouth while performing the exercises. This can also help with relaxation and stress management.
Repetitions and Sets
The number of repetitions and sets for exercises will vary depending on the individual's condition and progress. It is important to start with a low number of repetitions and gradually increase as tolerated. A general guideline is to aim for 10-15 repetitions per set, with 2-3 sets per exercise. It is important to listen to your body and not push yourself too hard, as this can worsen symptoms.
Progression of Exercises
As with any exercise program, it is important to progress gradually to avoid overexertion and injury. This is especially important for individuals with gastroparesis, as their condition may make it more difficult to tolerate intense physical activity. It is recommended to start with basic exercises and gradually increase difficulty by adding resistance or increasing the number of repetitions. It is important to consult with a physical therapist for guidance on proper progression of exercises.
Tips for Incorporating Exercises into Daily Routine
Consistency is key when it comes to pelvic physical therapy exercises for gastroparesis. It is important to find a routine that works for you and stick to it. This may involve setting aside a specific time each day for exercises or incorporating them into daily activities, such as while watching TV or during breaks at work. It may also be helpful to keep a journal to track progress and stay motivated. Remember to listen to your body and take breaks as needed.
Other Strategies for Managing Gastroparesis
Dietary Modifications
Gastroparesis is a condition that affects the stomach's ability to empty properly, leading to symptoms such as nausea, vomiting, and bloating. One of the most important strategies for managing gastroparesis is making dietary modifications. This includes eating smaller, more frequent meals, avoiding high-fat and high-fiber foods, and focusing on easily digestible options such as soups, smoothies, and pureed foods. It is also important to stay hydrated and limit or avoid alcohol and caffeine.
Medications
In addition to dietary changes, medications may also be prescribed to help manage symptoms of gastroparesis. These may include prokinetic agents, which help to stimulate stomach contractions and improve emptying, and antiemetics, which can help to reduce nausea and vomiting. It is important to work closely with a healthcare provider to find the right medication and dosage for each individual's specific needs.
Stress Management Techniques
Stress can have a significant impact on digestive health, and for those with gastroparesis, it can exacerbate symptoms. Therefore, incorporating stress management techniques such as deep breathing, meditation, and gentle exercise can be beneficial in managing gastroparesis. It is also important to prioritize self-care and find ways to relax and reduce stress in daily life.
Importance of Maintaining a Healthy Weight
Maintaining a healthy weight is crucial for managing gastroparesis. Being underweight can lead to malnutrition and nutrient deficiencies, while being overweight can put additional strain on the digestive system. Working with a healthcare provider and a registered dietitian can help individuals with gastroparesis find a healthy weight and develop a balanced and nutritious eating plan.
Follow-up with Healthcare Provider
Regular follow-up with a healthcare provider is essential for managing gastroparesis. This allows for monitoring of symptoms and adjustments to treatment plans as needed. It is also important to communicate any changes or concerns with the healthcare provider, as they can provide guidance and support in managing the condition.
If you are experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment