Back
Exploring the Intriguing Connection Between Headaches and Pelvic Floor Dysfunction
By Shannon Strauch, PTA, STMT-1 on 2/21/2024

Introduction: Headaches and pelvic floor dysfunction might seem like two unrelated health issues, but surprising as it may sound, there exists a fascinating connection between the two. While headaches are commonly associated with factors like stress, tension, or migraines, pelvic floor dysfunction involves a range of disorders affecting the muscles, ligaments, and connective tissues in the pelvic region. In recent years, research has shed light on the intriguing relationship between these seemingly disparate conditions, unraveling a complex interplay that warrants attention and exploration.
Understanding Pelvic Floor Dysfunction: The pelvic floor refers to a group of muscles and tissues that provide support to pelvic organs such as the bladder, uterus, and rectum. Dysfunction in this area can manifest in various forms, including pelvic pain, urinary incontinence, constipation, and sexual dysfunction. Causes of pelvic floor dysfunction are multifaceted, encompassing factors such as childbirth trauma, chronic constipation, prolonged sitting, pelvic surgery, and even psychological stress.
The Headache-Pelvic Floor Connection: While the precise mechanisms linking headaches and pelvic floor dysfunction are still being elucidated, several theories have emerged to explain their association:
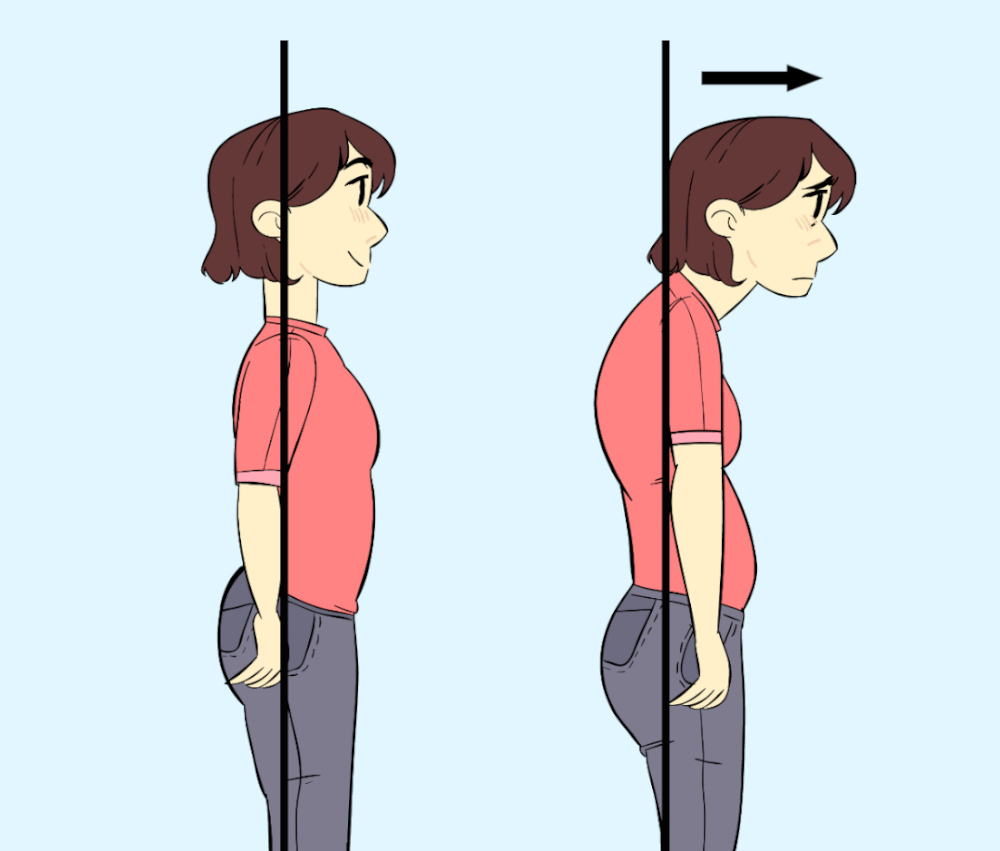
Muscular Tension: Both headaches and pelvic floor dysfunction involve muscular tension. Chronic stress or poor posture can lead to increased muscle tension not only in the neck and shoulders but also in the pelvic floor muscles. This interconnected tension may contribute to the development or exacerbation of headaches.
2. Central Sensitization: Central sensitization, a process in which the central nervous system becomes hypersensitive to pain signals, plays a crucial role in both headache disorders and pelvic pain syndromes. Shared neural pathways and neurotransmitter systems may underlie the co-occurrence of these conditions, amplifying pain perception and discomfort.
3. Dysfunctional Breathing Patterns: Dysfunctional breathing patterns, such as shallow or paradoxical breathing, are common in individuals with pelvic floor dysfunction. These aberrant breathing patterns can also trigger or exacerbate headaches by altering oxygen and carbon dioxide levels in the bloodstream and disrupting the balance of neurotransmitters involved in pain modulation.

4. Hormonal Influences: Hormonal fluctuations, particularly those related to the menstrual cycle, can influence both headaches and pelvic floor function. Changes in estrogen and progesterone levels may exacerbate pelvic pain and trigger migraines or tension headaches in susceptible individuals.
Clinical Implications and Treatment Approaches: Recognizing the interconnectedness of headaches and pelvic floor dysfunction is crucial for effective management and treatment. Integrative approaches that address both physical and psychological aspects of these conditions are often the most beneficial. Treatment modalities may include:
Pelvic floor physical therapy, which focuses on restoring muscle function and alleviating pelvic pain through exercises, manual therapy, and relaxation techniques.
Stress management strategies, such as mindfulness meditation, cognitive-behavioral therapy, and biofeedback, to reduce muscular tension and promote relaxation.
Addressing underlying factors contributing to both conditions, such as poor posture, sedentary lifestyle, dietary triggers, and hormonal imbalances.
Collaborative care involving healthcare providers from multiple disciplines, including physical therapists, urologists, gynecologists, neurologists, and pain specialists.
Conclusion: The intricate relationship between headaches and pelvic floor dysfunction underscores the importance of adopting a holistic approach to healthcare. By recognizing and addressing the interconnected factors contributing to both conditions, individuals can experience improved symptom management and enhanced quality of life. If you are dealing with both chronic headaches, chronic migraines, and chronic pelvic floor issues, contact us to find out more if there is an underlying connection
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment