Back
Hypermobility Disorders and Constipation: Why Can't I Poop?
By Shannon Strauch, PTA, STMT-1 on 4/10/2024
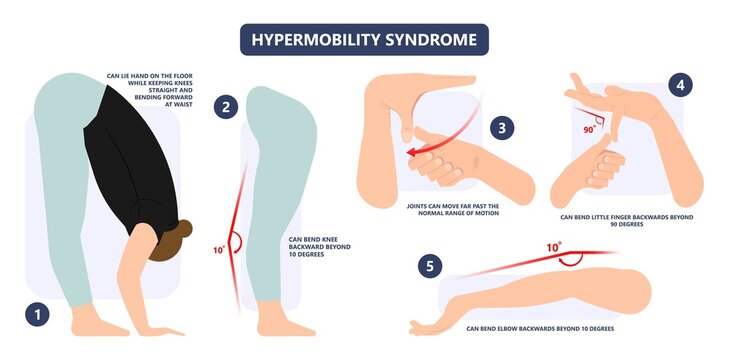
There are several types of hypermobility disorders, each characterized by excessive joint mobility and varying degrees of associated symptoms. Here are some common types:
Benign Joint Hypermobility Syndrome (BJHS):
This is a relatively mild form of hypermobility characterized by joint laxity without significant associated symptoms. Individuals with BJHS may have flexible joints that allow for a greater range of motion but typically do not experience severe joint pain or instability.Ehlers-Danlos Syndromes (EDS):
EDS refers to a group of genetic connective tissue disorders that affect collagen production, leading to hypermobility and other symptoms. The specific types of EDS include:Classical EDS:
Characterized by skin hyperextensibility, joint hypermobility, and easy bruising.
Hypermobility EDS:
Focuses primarily on joint hypermobility, often with joint pain, fatigue, and other related symptoms.
Vascular EDS:
Involves a higher risk of blood vessel and organ rupture due to weakened connective tissues.
Kyphoscoliotic EDS:
Affects joint hypermobility, muscle weakness, and curvature of the spine (kyphoscoliosis).
Arthrochalasia EDS:
Involves severe joint hypermobility and congenital hip dislocations.
Marfan Syndrome:
While primarily known for its impact on the cardiovascular system, Marfan syndrome can also cause joint hypermobility. It is caused by mutations in the FBN1 gene, leading to abnormalities in connective tissue.Joint Hypermobility Syndrome (JHS):
Similar to BJHS, JHS is characterized by joint hypermobility without significant structural abnormalities or associated conditions. It may involve joint pain, fatigue, and a higher risk of musculoskeletal injuries.Other Connective Tissue Disorders:
In addition to the above, there are other rare connective tissue disorders that can present with hypermobility as a prominent feature, such as Stickler syndrome, Loeys-Dietz syndrome, and Osteogenesis Imperfecta.
It's important to note that hypermobility can also occur as a secondary feature in conditions like rheumatoid arthritis, lupus, and certain neurological disorders. Proper diagnosis and management of hypermobility disorders typically involve a multidisciplinary approach with healthcare professionals such as rheumatologists, geneticists, physiotherapists, and occupational therapists.
Another common complaint of those with hypermobility disorders is constipation. Hypermobility can contribute to constipation through several mechanisms:
Pelvic Floor Dysfunction:
The pelvic floor muscles play a crucial role in bowel movements by contracting and relaxing to control the release of stool. In individuals with hypermobility, the pelvic floor muscles may be weaker or less coordinated, leading to difficulties in effectively emptying the bowels.Poor Posture and Alignment:
Hypermobility can affect posture and spinal alignment, which in turn can impact the function of the digestive system. Poor posture can compress the abdomen and pelvic area, potentially slowing down the movement of stool through the intestines.Connective Tissue Weakness:
Hypermobility is often associated with weak or lax connective tissues throughout the body. This weakness can extend to the digestive tract, causing reduced muscle tone and coordination in the intestines. As a result, peristalsis (the wave-like muscle contractions that move stool through the intestines) may be less efficient, leading to constipation.Nerve Impairment:
Hypermobility can sometimes be associated with nerve compression or dysfunction, especially in the lower back and pelvic region. Nerve issues can disrupt the signals that control bowel function, potentially causing constipation.Impact on Lifestyle Factors:
Hypermobility can affect daily activities and exercise routines. Reduced physical activity or limitations in certain movements due to hypermobility can contribute to a sedentary lifestyle, which is a known risk factor for constipation.Psychological Factors:
Chronic constipation can also be influenced by psychological factors such as stress, anxiety, or depression. Hypermobility-related challenges may contribute to psychological distress, which can further exacerbate constipation.
These factors can vary in their contribution to constipation depending on the individual's specific situation and the severity of their hypermobility. Addressing constipation in individuals with hypermobility often involves a comprehensive approach that addresses both the physical and psychological aspects of the condition. Pelvic Floor Physical Therapy can assess and address any muscle weakness, coordination or mechanics required in order to have more effective bowel movements. Contact us here at Pelvic Health 908-443-9880!
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment