Back
Is My Pain From Sciatica Or My Pelvic Floor?
By Dr. Christine Martirez PT, DPT on 4/16/2024

Sciatica and pelvic floor dysfunction causing pudendal nerve irritation are two distinct conditions that can impact pelvic health and overall well-being. In this blog post, we'll explore the anatomical pathways of the sciatic nerve and pudendal nerve, the muscles they innervate, and how pelvic floor physical therapy can aid in both diagnosis and treatment of these conditions.

Differentiating Sciatic Nerve Tightness and Pelvic Floor Dysfunction:
Anatomical Pathway and Function
Sciatic Nerve:
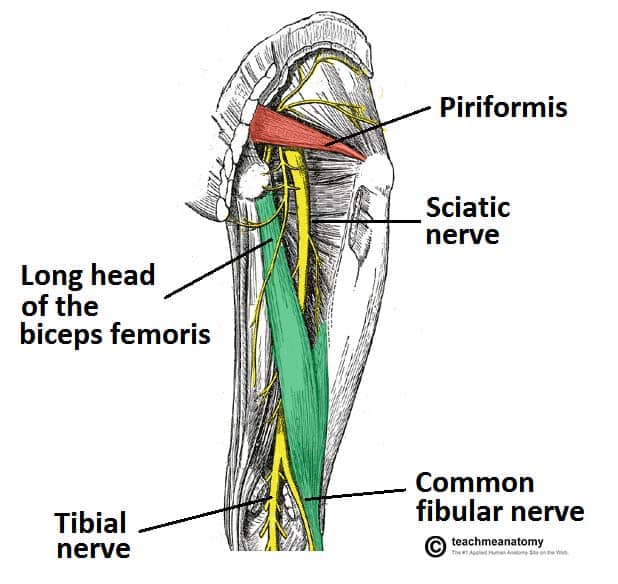
The sciatic nerve is the largest nerve in the body, originating from the lower lumbar and sacral nerve roots. It travels down the back of the thigh, branching into the tibial nerve and common peroneal nerve. The sciatic nerve primarily innervates the muscles of the posterior thigh (hamstrings), leg, and foot, providing sensation to these areas.Pudendal Nerve:
The pudendal nerve arises from the sacral nerve roots (S2-S4) and extends into the pelvic region. It innervates the muscles of the pelvic floor, including the external anal sphincter, urethral sphincter, and muscles of the perineum. The pudendal nerve also provides sensation to the genitals, perineum, and anus.
Muscle Innervation and Sensation
Sciatic Nerve:
Muscles innervated by the sciatic nerve include the hamstrings (biceps femoris, semitendinosus, semimembranosus), as well as muscles of the lower leg and foot (calf muscles, foot flexors, and extensors). The sciatic nerve does not directly innervate the pelvic floor muscles.Pudendal Nerve:
The pudendal nerve plays a crucial role in pelvic floor function, controlling the muscles involved in urinary and fecal continence, sexual function, and supporting pelvic organs. It also provides sensation to the genital region, perineum, and anus.
Symptoms of Sciatica
Radiating Pain:
Sciatica typically presents as a sharp, shooting pain that radiates from the lower back down one leg. The pain may travel along the path of the sciatic nerve, extending to the buttock, thigh, and even the foot.Numbness or Tingling:
Individuals with sciatica may experience numbness, tingling, or a pins-and-needles sensation in the affected leg. This can be accompanied by muscle weakness or difficulty moving the leg.Aggravated by Movement:
Symptoms of sciatica often worsen with certain movements or activities, such as sitting for prolonged periods, bending forward, or lifting heavy objects.Back Pain:
Sciatica is commonly associated with lower back pain, which may be dull or achy and localized to the lumbar spine or buttock area.
Symptoms of Pudendal Nerve Irritation or Pudendal Neuralgia
Pelvic and Posterior Chain Pain:
Pudendal neuralgia or irritation is characterized by chronic, sharp, or burning pain in the pelvic region, including the genitals, perineum (area between the anus and genitals), and rectum. This can also refer pain or paresthesia to the low back, buttocks, legs and feet.Pain with Sitting:
Individuals with pudendal neuralgia or irritation often experience increased pain while sitting, especially on hard surfaces. This discomfort may feel like a stabbing sensation or pressure in the pelvic area.Painful Sexual Intercourse:
Pudendal neuralgia or irritation can cause pain during sexual activity (dyspareunia), affecting intimacy and quality of life for affected individuals.Urinary or Fecal Symptoms:
Some people with pudendal neuralgia or irritation may experience urinary urgency, frequency, or hesitancy, as well as bowel dysfunction (such as constipation or difficulty with bowel movements).
Role of Pelvic Floor Physical Therapy
Diagnosis:
Pelvic floor physical therapists specialize in assessing and diagnosing pelvic floor dysfunction, which may include pudendal nerve entrapment or irritation. Through a comprehensive evaluation, therapists can identify muscle tightness, weakness, postural deficits, or neuromuscular dysfunction contributing to symptoms.Treatment Options:
Sciatic Nerve Tightness:
Pelvic floor physical therapy can address secondary effects of sciatic nerve tightness, such as compensatory pelvic floor muscle tension. Therapists may incorporate stretching, myofascial release, and nerve mobilization techniques to alleviate symptoms and improve mobility.Pelvic Floor Dysfunction:
For issues related to pudendal nerve dysfunction and pelvic floor disorders, pelvic floor physical therapy offers targeted interventions. Treatment may include pelvic floor muscle relaxation techniques, biofeedback training, therapeutic exercises, and lifestyle modifications, and more.
Seeking Comprehensive Care for Pelvic Health
Understanding the differences between sciatica and pelvic floor dysfunction is crucial for effective management of pudendal nerve-related issues. If you're experiencing symptoms such as pelvic pain, urinary or fecal incontinence, or sexual dysfunction, consider consulting with a pelvic floor physical therapist for specialized assessment and tailored treatment. With personalized interventions and comprehensive care, you can regain pelvic health and improve overall quality of life. Don't hesitate to prioritize your pelvic well-being and seek professional guidance for optimal recovery.
Suffering from sciatica or pudendal nerve irritation? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment