Back
Male Infertility: Premature Ejaculation
By Pelvic Health Physical Therapy on 2/2/2024

Welcome to my 4th and final segment of the male infertility series!
Now to recap: Infertility is a major public health issue, affecting about 15% of couples of reproductive ages. The male factor is involved in approximately 40-50% of these cases. Infertility is defined as the inability to conceive within a certain period, typically a year. However, infertility can have many factors involved such as: sperm pathologies, blockage of a duct, presence of pain, fracture of the penis, difficulty with ejaculation, anatomical defects, and even psychological issues. Treatment of male infertility may include therapies to target specific diagnoses (surgical or medical), medications to improve spermatogenesis (production of sperm), or artificial reproductive techniques to bypass reproductive barriers in the female partner.
Premature ejaculation is the most prevalent male sexual disorder. Regarding the definition of premature ejaculation, three criteria should be evaluated—short ejaculatory latency, concomitant distress, or a lack of sexual satisfaction and self-efficacy regarding the condition. There are two types of premature ejaculation: lifelong and acquired. The International Society for Sexual Medicine defines premature ejaculation as a sexual dysfunction characterized by ejaculation which always or nearly always occurs before or within about 1 minute of vaginal penetration, and the ability to delay ejaculation on or nearly all vaginal penetrations, and negative personal consequences, such as stress, bother, frustration, and/or avoidance of sexual intimacy. Others have defined premature ejaculation as a condition in which the subject lacks voluntary control over the muscles that regulate the ejaculation reflex.
In acquired premature ejaculation, males experience ejaculations occurring too soon after normal ejaculatory delay. The onset may be sudden or gradual, due to urological disorders (urinary incontinence), thyroid dysfunction (hypothyroidism or hyperthyroidism), psychological (especially abuse), or a combination of these factors.
Biological factors that can also contribute or cause premature ejaculation:
Abnormal hormone levels;
Abnormal levels of brain chemicals called neurotransmitters;
Inflammation and infection of the prostate or urethra;
Inherited traits.
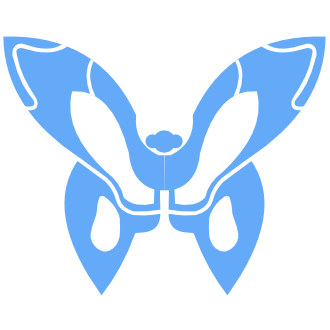
Having premature ejaculation doesn’t mean there’s anything wrong with the sperm. It may mean that certain muscles of the pelvic floor might be involved, including:
Bulbospongiosus
Puborectalis
Genitourinary sphincter
If one of the muscles are tightened or have the inability to contract, they may disrupt the ability to control the ejaculation reflex, thus unable to prolong latency.
Pelvic Floor Physical Therapy can help, especially with:
Training patients to recognize how and when to control the muscles involved in ejaculation control and for strengthening the muscles of the perineal floor.
Achieving muscle contraction to improve awareness of motor activity via Kegels and reverse Kegels.
Assisting with achieving adequate muscle contraction, especially with the perineal muscles and genitourinary sphincter via biofeedback.
Electric stimulation of perineal floor to directly stimulate the pudendal nerve, resulting in stimulation of the puborectalis which causes the urethral sphincter to contract.
Discussing the need to experiment with different sexual positions.
Discussing lifestyle modifications (eg: cessation of smoking, eating a healthy diet that includes lots of fiber and water, sleeping 7-9 hours per night, initiating daily regular exercise).
Discussing the need to refer to appropriate resources (eg: urology, sex therapists, general clinical psychology, etc.).
If you’re experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Works Cited:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5904846/pdf/RMB2-11-59.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4003840/pdf/10.1177_1756287214523329.pdf
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment