Back
Male / Transgender / Transmale / Transfemale Sexual Pelvic Floor Dysfunction and Chronic Opioid Use
By Pelvic Health Physical Therapy on 2/2/2024
All humans can suffer from sexual dysfunction at some point in their lives. Different reasons can lead to issues with sexual desire, premature ejaculation, erectile dysfunction, amenorrhea (lack of menstrual cycle), and anovulation (lack of ovulation). Sexual dysfunction can arise from many physical factors such as heart disease, high cholesterol, high blood pressure, diabetes, obesity, and smoking. On the other hand, depression, anxiety, stress, relationship problems, and other mental health concerns can also interfere with sexual feelings.
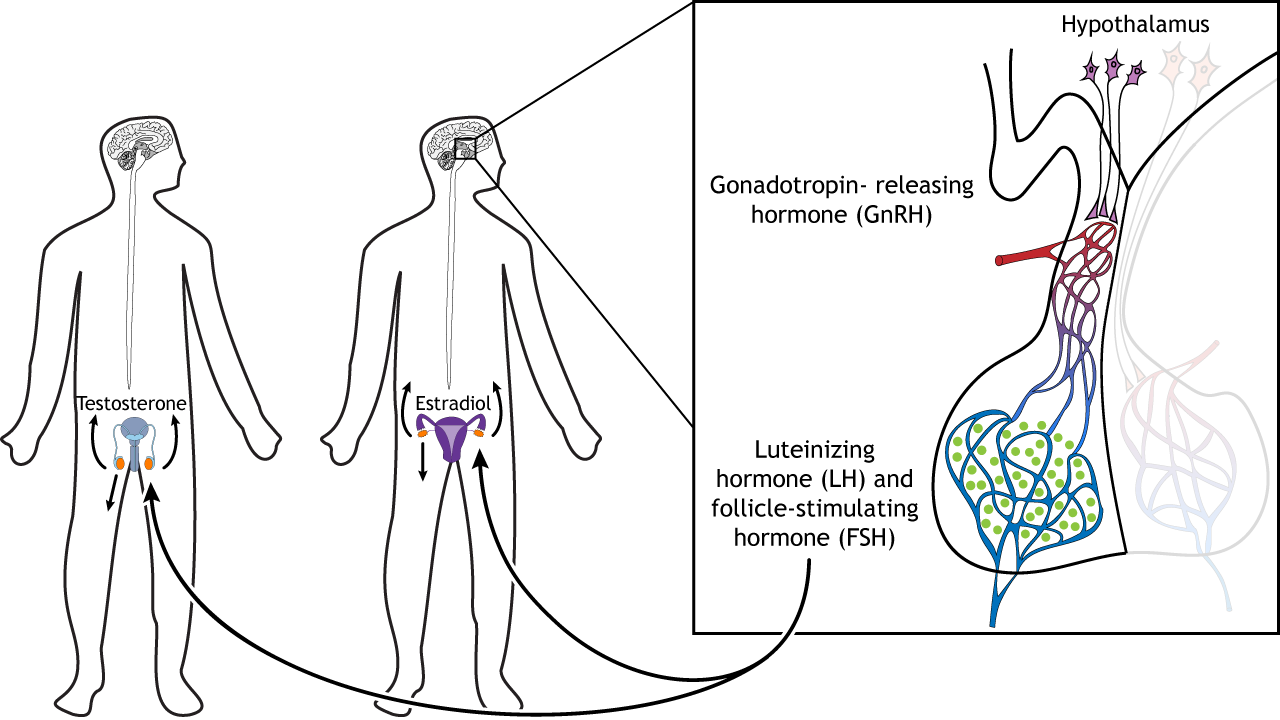
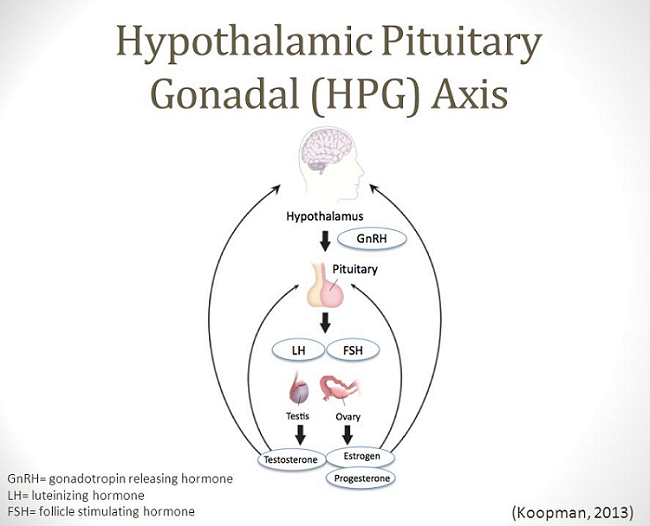
Today, we are focusing on medication use and how it can affect sexual functioning. Why does it matter? For any gender identity, chronic opioid use following gender affirming surgery, prostatectomy, and other procedures to treat pelvic floor pain has been linked to influencing parts of your brain that control sexual desire and function such as the: hypothalamus, pituitary gland, and gonadal glands (e.g.: testes and ovaries) - also known as the hypothalamic-pituitary-gonadal axis (see picture below). Chronic opioid use has been shown to reduce the release of gonadotrophin releasing hormone (GnRH), which in turn reduces follicle stimulating hormone (FSH) and luteinizing hormone (LH) which influences ovary and teste function.
So, what can Pelvic Floor Physical Therapy do to help?
A Pelvic Floor Therapist helps identify faulty movement patterns adapted after your surgery
We perform soft tissue and scar tissue mobilization to improve mobility and decrease pain/hypersensitivity
We teach proper breathing patterns to help your pelvic floor function better
We identify and manage external stressors (e.g.: work stress, relationship stress)
How can Pelvic Floor Physical Therapy help?
Soft tissue and surgical scar tissue mobilization relaxes muscle tension and reduces overall tightness, adhesions, and pain
Biofeedback improves muscle coordination and neurological response
Dry needling supports the relaxation of muscle tightness in the perineum and other areas to improve pain response
Manual, therapeutic, and exercise techniques in the office and at home allow for overall improved pain management (lower back, hips, abdomen, pelvic floor)
Visceral (organ) mobilization leads to improved urinary and bowel function
If you’re experiencing pelvic pain or dysfunction and are medically clear to begin physical therapy, please reach out to us here at the Pelvic Health Center in Madison, NJ to set up an evaluation & assessment! Feel free to call us 908-443-9880 or email us at contact@pelvichealthnj.com.
Read More:
Exercise to reduce pelvic floor dysfunction associated with childbirth?? By Amalie Malka Flamm on 7/25/2024 What exercises can help reduce pelvic floor dysfunction associated with childbirth? Why does my taint hurt (male)? By Shannon Strauch, PTA, STMT-1 on 7/24/2024 Where is your perineum, what is it's function, and why do you have pain?
Are you ready to live pain free?
Request An Appointment