Back
Managing Bacterial Vaginosis and Constipation: Are the Two Conditions Related?
By Pelvic Health Physical Therapy on 2/2/2024
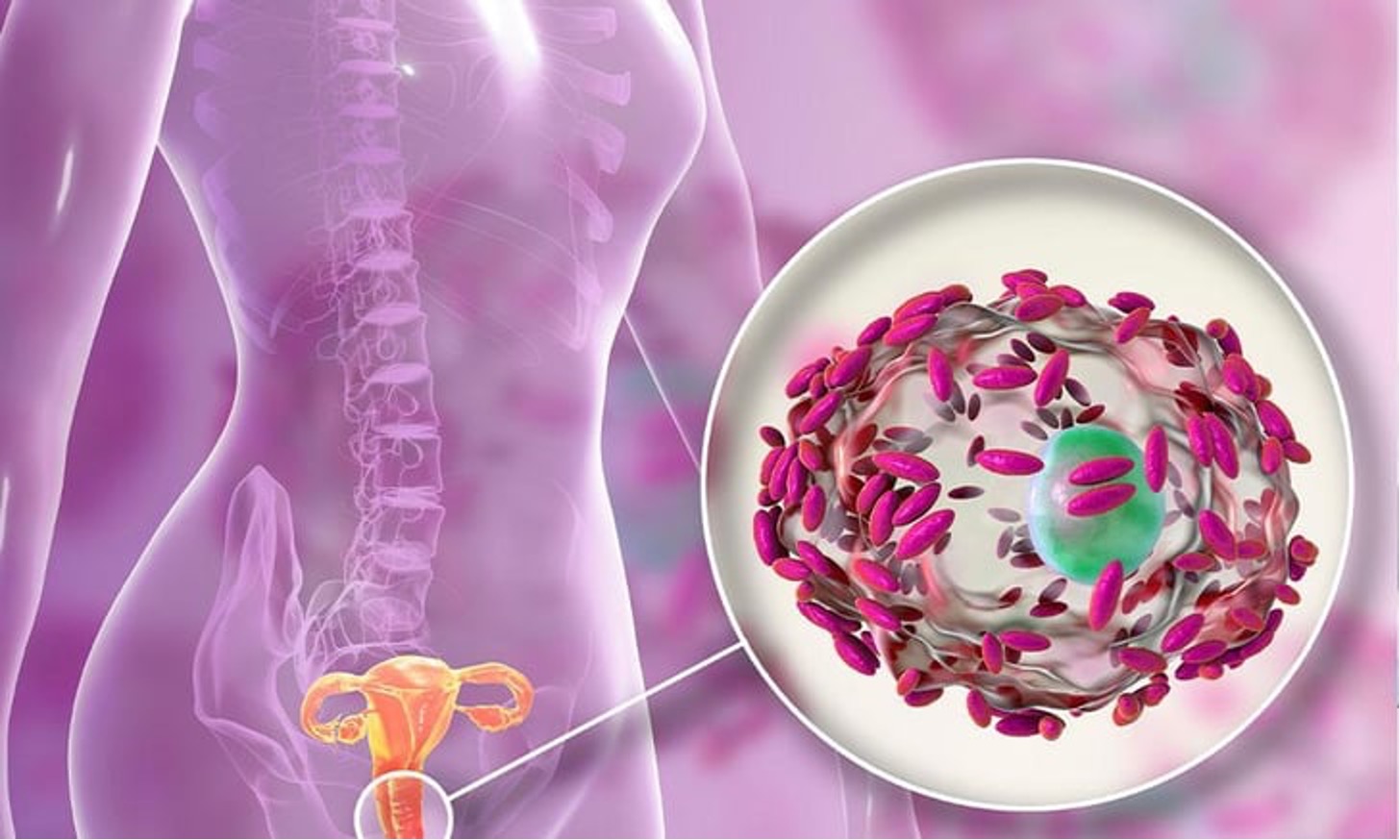
What is Bacterial Vaginosis?
Bacterial vaginosis is a common vaginal infection caused by an imbalance in the bacterial ecosystem of the vagina. In a healthy vagina, there is a delicate balance between various types of bacteria, including beneficial bacteria (Lactobacillus) and potentially harmful bacteria. When this balance is disrupted, it can lead to bacterial vaginosis.
Key Features of Bacterial Vaginosis Include:
1. Microbial Imbalance:
The normal balance of bacteria in the vagina is disrupted, and there is an overgrowth of harmful bacteria, such as Gardnerella vaginalis, Prevotella, and others, while the levels of Lactobacillus species decrease.2. Symptoms:
bacterial vaginosis may not always cause noticeable symptoms, but when present, common symptoms include a thin, grayish-white vaginal discharge with a distinct fishy odor. The odor may become more noticeable after sexual intercourse.3. Discharge:
The vaginal discharge in bacterial vaginosis is different from the discharge seen in yeast infections. It is typically watery, thin, and may have an unpleasant odor (eg: fishy odor).4. Itching or Irritation:
Some women with bacterial vaginosis may experience mild itching or irritation in the genital area, but these symptoms are not as prominent as they are in other vaginal infections like yeast infections.5. Risk Factors:
Certain factors can increase the risk of developing bacterial vaginosis, including multiple sexual partners, douching, a new sexual partner, or using intrauterine devices (IUDs) for contraception.6. Complications:
While bacterial vaginosis is usually not a serious condition if left untreated, it may increase the risk of complications such as pelvic inflammatory disease (PID), preterm birth in pregnant women, and increased susceptibility to sexually transmitted infections (STIs).Diagnosis of bacterial vaginosis is typically based on a combination of clinical symptoms, examination of vaginal discharge, and laboratory tests. Treatment often involves antibiotics, such as metronidazole or clindamycin, which help restore the balance of bacteria in the vagina. It's important for individuals experiencing symptoms or suspecting they have bacterial vaginosis to seek medical attention for proper diagnosis and appropriate treatment.
How are Bacterial Vaginosis and Constipation Related?
Bacterial vaginosis and constipation are two separate health conditions, but there is some evidence to suggest that they may be linked indirectly through factors such as the gut microbiome.
1. Gut Microbiome
: Both bacterial vaginosis and constipation can be influenced by the balance of bacteria in the gut. The gut microbiome plays a crucial role in maintaining overall health, including the health of the reproductive system. Disruptions in the balance of bacteria in the gut can potentially affect the vaginal microbiota as well.2. Immune System
: The gut is a significant part of the immune system. Changes in the gut microbiome and immune system function can impact susceptibility to infections, including those in the vaginal area.3. Diet and Lifestyle Factors
: Diet and lifestyle can contribute to both constipation and bacterial vaginosis. For example, a diet low in fiber and high in processed foods may contribute to constipation and alter the gut microbiome. Additionally, factors such as stress can affect both conditions.4. Antibiotic Use
: Antibiotic use is a potential factor that could be linked to both bacterial vaginosis and constipation. Antibiotics can disrupt the balance of bacteria in the gut, leading to constipation, and may also contribute to changes in the vaginal microbiota.Other Considerations when Managing Bacterial Vaginosis and Constipation.
Managing bacterial vaginosis and constipation involves a combination of lifestyle modifications, medical interventions, and preventive measures. Here are some considerations for managing each condition:
Bacterial Vaginosis:
Antibiotics:
Bacterial vaginosis is commonly treated with antibiotics like metronidazole or clindamycin. It's crucial to complete the full course of antibiotics as prescribed by a healthcare professional.
Probiotics:
Probiotics, especially those containing Lactobacillus strains, may help restore the balance of bacteria in the vagina. They can be taken orally or used as vaginal suppositories.
Avoidance of Irritants:
Avoid using harsh soaps, douches, or scented products in the genital area, as they can disrupt the natural balance of bacteria.
Safe Sex Practices:
Practicing safe sex, including using condoms, can reduce the risk of introducing new bacteria into the vagina.
Regular Gynecological Check-ups:
Regular check-ups with a healthcare provider are important, especially for women who experience recurrent bacterial vaginosis. This helps monitor and manage the condition effectively.
Constipation:
Dietary Changes:
Increase dietary fiber intake by consuming more fruits, vegetables, whole grains, and legumes. Fiber adds bulk to the stool and helps promote regular bowel movements.
Hydration:
Drink plenty of water to prevent dehydration, as it helps soften the stool and makes it easier to pass.
Regular Exercise:
Engage in regular physical activity, as it stimulates bowel movements and helps maintain a healthy digestive system.
Establish Regular Bowel Habits:
Respond to the body's natural signals for bowel movements. Avoid delaying or ignoring the urge to have a bowel movement.
Probiotics:
Probiotics may help regulate gut health and improve bowel regularity. They can be found in certain foods (yogurt, kefir) or taken as supplements.
Avoidance of Certain Medications:
If constipation is related to medication, consult with a healthcare professional to explore alternative options or strategies.
Biofeedback and Pelvic Floor Therapy:
In some cases, especially for chronic constipation, biofeedback or pelvic floor therapy may be recommended to improve muscle coordination and function.
Laxatives (Short-term Use):
In certain situations, healthcare providers may recommend short-term use of laxatives. However, their prolonged use without medical supervision is not advised.
It's important to note that while there may be some indirect connections between these two conditions, they are not directly causative of each other. Both conditions have their own set of causes, risk factors, and treatments.
Open communication with a healthcare provider is crucial for managing bacterial vaginosis and constipation. They can provide personalized treatment recommendations, monitor symptoms, and address any concerns or questions. It is important to be honest and open about symptoms and any changes in health to ensure proper treatment and management of these conditions.
If you are experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
How Visceral Mobilization Can Assist with the Treatment of SIBO By Dr. Christine Martirez PT, DPT on 10/22/2024 Learn about SIBO and how visceral mobilizations can be an integral part of your recovery journey Understanding Sacral Pain and How Pelvic Floor Therapy Can Help By Dr. Christine Martirez PT, DPT on 10/21/2024 Learn about sacral pain & how pelvic floor therapy can be an intregral part of your healing journey
Are you ready to live pain free?
Request An Appointment