Back
Overactive Bladder?
By Shannon Strauch, PTA, STMT-1 on 5/3/2024
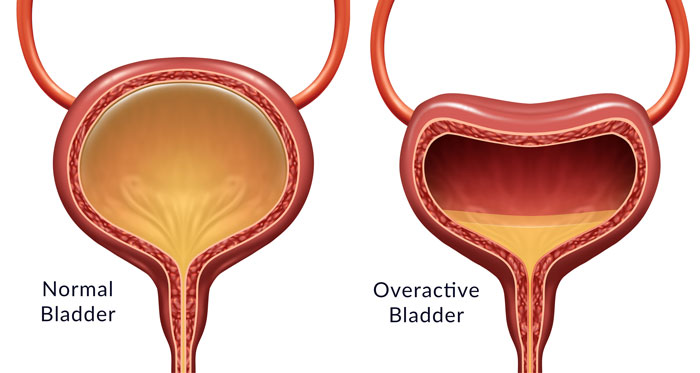
Bladder urgency frequency (BUF) refers to the frequent and intense urge to urinate, often accompanied by leaking or incontinence. This condition can significantly impact daily life, causing disruptions to work, social activities, and sleep. It is essential to understand the causes of BUF, which can include urinary tract infections (UTIs), overactive bladder (OAB), bladder irritation, nerve damage, and pelvic floor dysfunction.
Pelvic floor physical therapy (PFPT) is a valuable treatment option for BUF. PFPT targets the muscles, nerves, and connective tissues of the pelvic floor to improve function and reduce symptoms. Techniques such as pelvic floor exercises (Kegels), biofeedback, electrical stimulation, and manual therapy can be used to enhance bladder control and reduce urgency and frequency.
The benefits of PFPT for BUF include increased bladder control, reduced urgency and frequency, improved pelvic floor muscle strength and coordination, and enhanced quality of life. PFPT takes a holistic approach, addressing underlying issues and promoting overall pelvic health.
Managing BUF also involves lifestyle modifications, stress management strategies, and proper toileting habits. Seeking professional evaluation and considering PFPT can be proactive steps towards managing BUF and improving pelvic health.
Pelvic Floor Tightness and Bladder Urgency:
Pelvic floor tightness refers to increased tension or stiffness in the muscles of the pelvic floor, which can affect bladder function.
When the pelvic floor muscles are tight, they may not relax properly during urination, leading to incomplete emptying of the bladder and a sensation of urgency.
Symptoms:
Bladder urgency: Individuals with pelvic floor tightness may experience a frequent and intense urge to urinate, even when the bladder is not full.
Difficulty starting or stopping urination: Tight pelvic floor muscles can interfere with the normal urinary flow, causing difficulties in initiating or stopping urination.
Pelvic pain: Some people may also experience pelvic pain or discomfort, which can worsen with activities like sitting for prolonged periods or during intercourse.
Diagnosis:
Healthcare providers, such as urologists or pelvic floor physical therapists, can conduct assessments to evaluate pelvic floor muscle function and identify areas of tightness.
Diagnosis may involve a physical examination, pelvic floor muscle assessment, and possibly imaging studies or electromyography (EMG) to assess muscle activity.
Treatment Approaches:
Pelvic Floor Physical Therapy (PFPT):
A specialized PFPT program is often the primary treatment for pelvic floor tightness and associated bladder urgency. PFPT can include techniques such as:Pelvic floor exercises to strengthen and relax the pelvic floor muscles.
Manual therapy, including massage and stretching techniques, to release tension and improve muscle flexibility.
Biofeedback to help patients gain awareness and control over pelvic floor muscle activity.
Relaxation Techniques:
Incorporating relaxation techniques such as deep breathing, progressive muscle relaxation, and mindfulness practices can also help reduce pelvic floor tension and alleviate urgency symptoms.
Bladder Training:
Working with a healthcare provider on a bladder training program can help improve bladder control and reduce urgency episodes.
Medication:
In some cases, medications that relax the bladder or pelvic floor muscles may be prescribed to manage urgency symptoms temporarily.
Lifestyle Modifications:
Lifestyle changes like managing stress levels, maintaining a healthy weight, staying hydrated, and avoiding bladder irritants (such as caffeine, alcohol, and certain foods) can support bladder health and complement treatment efforts.
If you're experiencing bladder urgency due to pelvic floor tightness, consulting with a healthcare provider specializing in pelvic floor dysfunction or PFPT is recommended. They can assess your condition, develop a personalized treatment plan, and provide guidance on managing symptoms effectively.
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment