Back
Pelvic Floor Physical Therapy for Pelvic Organ Prolapse: Understanding Causes and Treatments
By Pelvic Health Physical Therapy on 2/2/2024
Pelvic organ prolapse is the descent of one or more areas of the anterior vaginal wall, posterior vaginal wall, uterus (cervix), or apex of the vagina. Pelvic organ prolapse occurs in a small percentage of women and is usually detected during a vaginal exam by an OBGYN. Pelvic organ prolapse surgery is required for an even smaller percentage of cases. However, most of those cases are typically women between ages 60 and 69.
General symptoms of pelvic organ prolapse include:
Vaginal bulging;
Pelvic (or rectal) pressure;
Low back pain;
Bleeding, discharge, infection;
Splinting / digitation (use of fingers to press on posterior vaginal wall to assist with defecation);
Reduced symptoms with gravity reduced positions (stacking pillows under the buttocks, legs elevated on wall);
Symptoms are more prominent with straining.
Older females are most often at risk to developing pelvic organ prolapse due to reduced collagen levels or disease, childbirth-related PFM trauma, and/or hyperflexibility; however, pelvic organ prolapse is often associated with:
Collagen defects/disease (eg: Ehlers-Danlos syndrome, Marfan syndrome, other connective tissue disorders);
Loss of nerve muscle, ligament, or fascial integrity;
Race - Caucasian race more likely to have prolapse;
Menopause - estrogen deficiency leads to thinning of the supportive connective tissue;
Pelvic surgery (eg: hysterectomy);
Traumatic childbirth;
Raised intra-abdominal pressure (eg: COPD, straining, constipation, heavy lifting).
The development of pelvic organ prolapse may be due to:
Underactive pelvic floor muscles;
Overactive pelvic floor muscles;
Non-functioning pelvic floor muscles.
What are the types of pelvic organ prolapse?
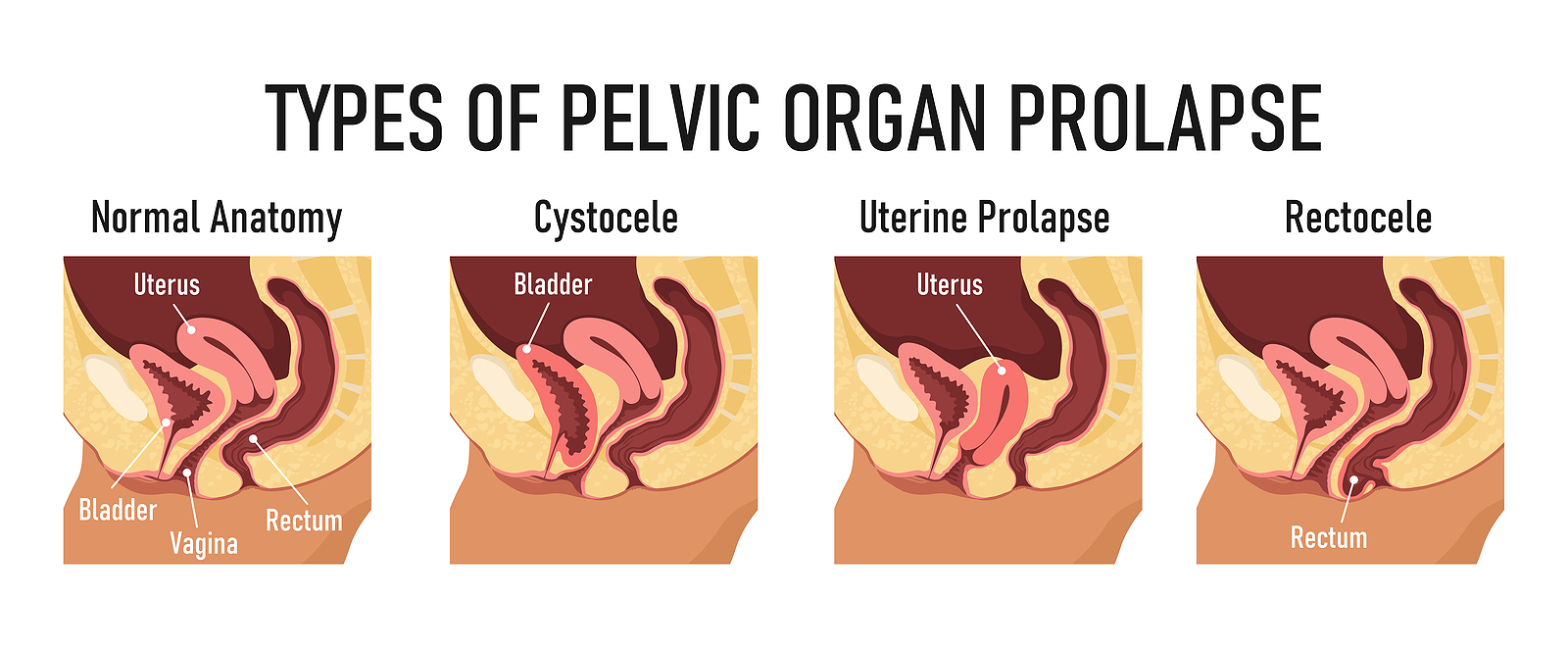
There are several different types of pelvic organ prolapses. When describing pelvic organ prolapses, they go by anatomy/organ (eg: cystocele - bladder, rectocele - rectum), by change (eg: herniation, prolapse, protrusion, relaxation), and by position (eg: anterior or posterior).
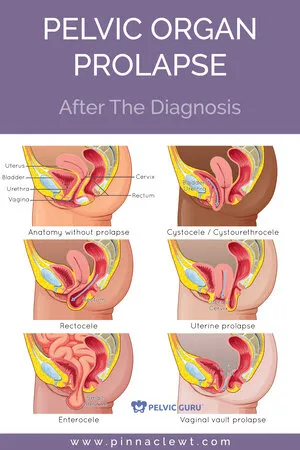
The types of pelvic organ prolapse include:
Posterior wall compartment or rectocele (prolapse of the rectum) – This type of vaginal prolapse involves a prolapse of the posterior wall of the vagina. When this wall weakens, the rectal wall pushes against the vaginal wall, creating a bulge. This bulge may become especially noticeable during bowel movements.
Symptoms include:
Vaginal pressure or discomfort;
Protrusion from posterior vaginal wall;
Need to reposition during bowel movement, also called incomplete emptying;
Difficulty with evacuation rectum with use of splinting (pressing the back of the vaginal wall to assist with evacuation).
Anterior wall compartment or cystocele (prolapse of the bladder, bladder drop) - this can occur when the anterior wall of the vagina (pubocervical fascia) prolapses. As a result, the bladder may prolapse into the vagina. When this condition occurs, the urethra usually prolapses as well. A urethral prolapse is called a urethrocele. When both the bladder and urethra prolapse, this condition is known as a cystourethrocele.
Poor or prolonged urinary stream;
Feeling of incomplete emptying;
Positional changes to start or complete emptying;
Stress urinary incontinence;
Urinary retention with obstruction;
When a patient has a urethrocele, they oftentimes experience dribble post micturition (after urination).
Enterocele middle compartment (herniated small bowel) - the weakening of the upper vaginal supports can cause this type of vaginal prolapse. This condition primarily occurs following a hysterectomy. An enterocele results when the front and back walls of the vagina separate, allowing the intestines to push against the vaginal skin.
Symptoms include:
Pelvic or vaginal pressure;
Difficulty evacuating rectum and / or emptying bladder;
Lower back discomfort that worsens as the day progresses;
Increased discomfort with prolonged standing, relieved with lying down.
Uterine prolapse middle compartment - this involves a weakening of a group of ligaments called the uterosacral ligaments at the top of the vagina. This causes the uterus to fall, which commonly causes both the front and back walls of the vagina to weaken as well.
This condition is broken down into 4 stages:
First-degree prolapse: The uterus droops into the upper portion of the vagina.
Second-degree prolapse: The uterus falls into the lower part of the vagina.
Third-degree prolapse: The cervix, which is located at the bottom of the uterus, sags to the vaginal opening and may protrude outside the body.
Fourth-degree prolapse: The entire uterus protrudes entirely outside the vagina. This condition is also called complete prolapse.
Symptoms include of uterine prolapse would include:
Blood-stained purulent discharge;
Difficulty in bowel or bladder emptying;
Low back pain or discomfort that worsens as the day progresses;
Increased discomfort with prolonged standing, relieved with laying down.
Vaginal vault prolapse - this type of prolapse may occur following a hysterectomy, which involves the removal of the uterus. Because the uterus provides support for the top of the vagina, this condition is common after a hysterectomy, with upwards of 10% of women developing a vaginal vault prolapse undergoing a hysterectomy. In vaginal vault prolapse, the top of the vaginal gradually falls toward the vaginal opening. This may cause the walls of the vagina to weaken as well. Eventually, the top of the vagina inside out. A vaginal vault prolapse often accompanies an enterocele.
Evaluation would include:
Thorough past medical history;
Quantification of prolapse (ie: grading severity of prolapse);
Screen cardiovascular, pulmonary, renal and cognitive disorders;
General orthopedic examination (eg: hip and lumbar spine range of motion, strength assessment, flexibility assessment, etc.);
Pelvic examination;
Possible urodynamics, defecography, or MRI (prescribed by a gynecologist or urologist).
Usually treated:
Pelvic floor strengthening and/or stretching via manual therapy and therapeutic exercise;
Biofeedback training for the patient to learn which pelvic floor muscles to contract and relax;
Bladder retraining to extend time with voiding;
Electrical stimulation to help ease pain.
Pelvic organ prolapse can also be treated with a pessary that is prescribed by a gynecologist. A pessary is a device inserted non-surgically into the vagina to reduce prolapse, prove support, and relieve pressure on the bladder and bladder. Made of silicone, many are ring-shaped. Optional for those who are not surgical candidates and is considered minimally invasive. May be as effective as surgery in improving health-related quality of life. Potential benefits include improved symptoms of bulging, decreased bladder irritation, and improved body self-image. Complications of pessary insertion may include bleeding, vaginal discharge, pain, constipation, and/or odor; although severe complications are rare.
If you’re experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Works Cited:
Read More:
How Visceral Mobilization Can Assist with the Treatment of SIBO By Dr. Christine Martirez PT, DPT on 10/22/2024 Learn about SIBO and how visceral mobilizations can be an integral part of your recovery journey Understanding Sacral Pain and How Pelvic Floor Therapy Can Help By Dr. Christine Martirez PT, DPT on 10/21/2024 Learn about sacral pain & how pelvic floor therapy can be an intregral part of your healing journey
Are you ready to live pain free?
Request An Appointment