Back
Pelvic Organ Prolapse (POP)
By Shannon Strauch, PTA, STMT-1 on 1/9/2024
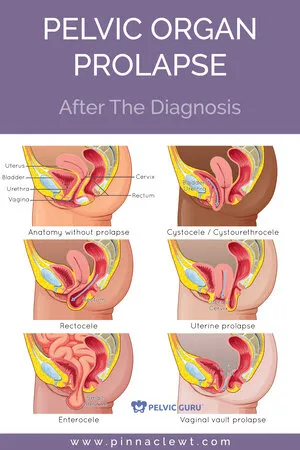
Pelvic organ prolapse (POP) occurs when one or more pelvic organs, such as the uterus, bladder, or rectum, protrude into or outside the vaginal canal due to weakened or damaged pelvic floor muscles and ligaments. The pelvic floor supports these organs, and when this support is compromised, it can lead to prolapse.
Common causes of pelvic organ prolapse include:
Childbirth:
The stretching and weakening of pelvic muscles during childbirth can contribute to pelvic organ prolapse, particularly if there were complications during delivery.Aging:
The natural aging process can result in a gradual weakening of the pelvic floor muscles and connective tissues.Hormonal Changes:
Reduced estrogen levels during menopause can lead to changes in pelvic tissues, contributing to prolapse.Chronic Straining:
Chronic constipation, heavy lifting, or activities that put excessive pressure on the pelvic floor can contribute to prolapse.Chronic Coughing
The symptoms of pelvic organ prolapse can vary depending on the organs involved and the severity of the condition. Common symptoms may include:
A feeling of fullness or pressure in the pelvic area
Discomfort or pain in the pelvic region
Bulging or protrusion from the vaginal opening
Difficulty with bowel movements or urinary incontinence
Sexual dysfunction
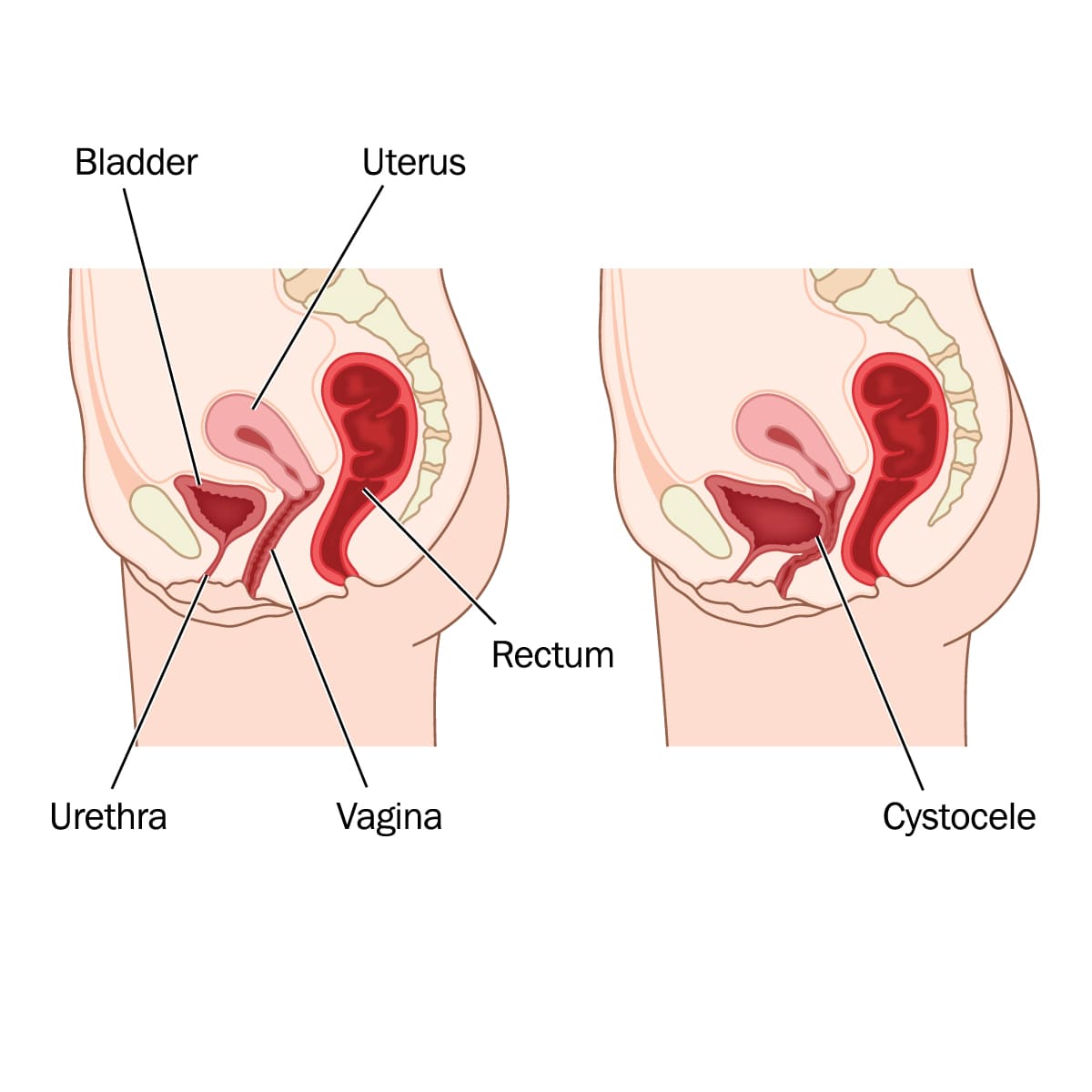
CYSTOCELE
A cystocele is a type of pelvic organ prolapse that specifically involves the bladder. In a cystocele, the supportive tissues between a woman's bladder and vaginal wall weaken, allowing the bladder to sag into the vagina. This condition is sometimes referred to as a prolapsed or dropped bladder.
Common causes of cystocele include:
Childbirth:
The process of giving birth, especially if it involves trauma to the pelvic floor muscles and tissues, can contribute to the development of a cystocele.Aging:
As women age, the natural weakening of muscles and tissues in the pelvic area can occur, increasing the risk of pelvic organ prolapse.Hormonal Changes:
Reduced estrogen levels, particularly during menopause, can lead to changes in the pelvic tissues, making them more susceptible to prolapse.Chronic Straining:
Activities that involve repeated heavy lifting, chronic constipation, or conditions that cause increased pressure in the pelvic area can contribute to a cystocele.
The symptoms of a cystocele can vary but may include:
A feeling of fullness or pressure in the pelvic area.
The sensation that something is bulging into the vaginal canal.
Problems with urination, such as difficulty emptying the bladder completely or urinary incontinence.
Discomfort or pain during sexual intercourse.
Treatment options for a cystocele depend on the severity of the symptoms and may include:
Pelvic Floor Physical Therapy:
Exercises and techniques aimed at strengthening the pelvic floor muscles can be beneficial.Lifestyle Modifications:
Maintaining a healthy weight, avoiding heavy lifting, and managing constipation can help prevent further strain on the pelvic floor.Pessaries:
These are devices inserted into the vagina to support the prolapsed organs.Hormone Replacement Therapy (HRT):
Estrogen replacement therapy may be considered for postmenopausal women.Surgery:
In more severe cases or when conservative measures are ineffective, surgical intervention may be recommended to repair and support the bladder and surrounding tissues.
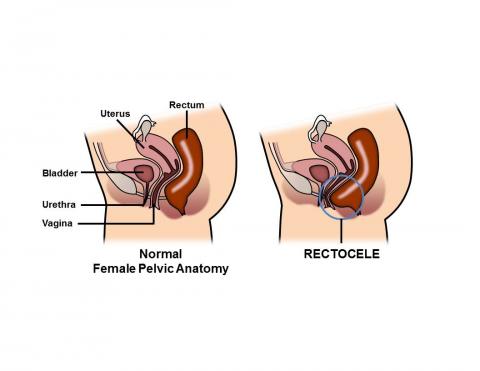
RECTOCELE
A rectocele is a type of pelvic organ prolapse that involves the rectum pushing into the back wall of the vagina. This condition occurs when the supportive tissues between the rectum and the vagina weaken, allowing the rectum to bulge into the vaginal canal.
Causes of rectocele can include:
Childbirth:
The strain on the pelvic floor muscles and tissues during childbirth, especially if there are complications or trauma, can contribute to the development of a rectocele.Aging:
As women age, the natural aging process can result in the weakening of pelvic muscles and connective tissues, making them more susceptible to prolapse.Hormonal Changes:
Reduced estrogen levels, particularly during menopause, can lead to changes in pelvic tissues, increasing the risk of prolapse.Chronic Straining:
Activities that involve repeated heavy lifting, chronic constipation, or conditions that cause increased abdominal pressure can contribute to the development of a rectocele.
Symptoms of rectocele may include:
A bulging sensation in the vagina, especially during bowel movements.
Discomfort or pain in the pelvic region.
Problems with bowel movements, such as difficulty emptying the rectum, constipation, or the need for manual assistance to evacuate stool.
Urinary incontinence or urinary dribble
Treatment options for rectocele depend on the severity of symptoms and may include:
Pelvic Floor Physical Therapy:
Exercises and techniques to strengthen the pelvic floor muscles.Lifestyle Modifications:
Maintaining a healthy weight, avoiding heavy lifting, and managing constipation can help prevent further strain on the pelvic floor.Pessaries:
Devices inserted into the vagina to support the prolapsed organs.Hormone Replacement Therapy (HRT):
Estrogen replacement therapy may be considered for postmenopausal women.Surgery:
In more severe cases or when conservative measures are ineffective, surgical intervention may be recommended to repair and support the pelvic organs.
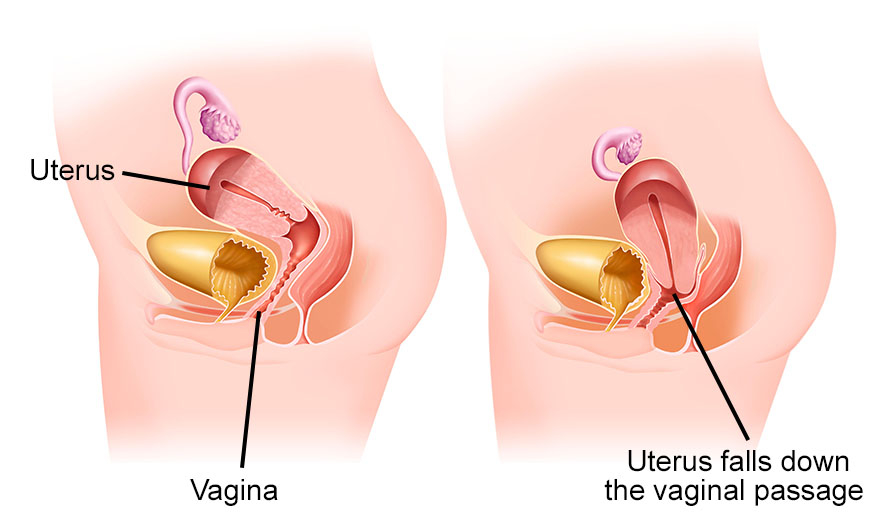
UTERINE PROLAPSE
Uterine prolapse is a condition in which the uterus descends from its normal position into the vagina or, in more severe cases, may protrude outside the vaginal opening. This happens when the muscles and ligaments that support the uterus weaken, allowing it to sag or move out of place.
Common causes of uterine prolapse include:
Childbirth:
The strain on the pelvic floor muscles and tissues during childbirth, especially multiple deliveries or difficult labor, can contribute to uterine prolapse.Aging:
As women age, hormonal changes and the natural aging process can result in the weakening of pelvic muscles and connective tissues, increasing the risk of prolapse.Hormonal Changes:
Reduced estrogen levels, particularly during menopause, can lead to changes in pelvic tissues, making them more susceptible to prolapse.Chronic Straining:
Activities that involve repeated heavy lifting, chronic constipation, or conditions that cause increased abdominal pressure can contribute to uterine prolapse.
Symptoms of uterine prolapse may include:
A feeling of fullness or pressure in the pelvic area.
The sensation of something protruding from the vaginal opening.
Discomfort or pain in the pelvic region.
Problems with urinary function, such as difficulty emptying the bladder or stress urinary incontinence.
Difficulty with bowel movements.
Treatment options for uterine prolapse depend on the severity of symptoms and may include:
Pelvic Floor Physical Therapy:
Exercises and techniques to strengthen the pelvic floor muscles.Lifestyle Modifications:
Maintaining a healthy weight, avoiding heavy lifting, and managing constipation can help prevent further strain on the pelvic floor.Pessaries:
Devices inserted into the vagina to support the prolapsed uterus.Hormone Replacement Therapy (HRT):
Estrogen replacement therapy may be considered for postmenopausal women.Surgery:
In more severe cases or when conservative measures are ineffective, surgical intervention may be recommended to repair and support the pelvic organs.
ENTEROCELE
An enterocele is a type of pelvic organ prolapse that involves the small intestine pushing into the vaginal space. This condition occurs when the supportive tissues between the vagina and the rectum weaken, allowing the small intestine to bulge into the vaginal canal.

Causes of enterocele can include:
Childbirth:
The strain on the pelvic floor muscles and tissues during childbirth, especially if there are complications or trauma, can contribute to the development of an enterocele.Aging:
As women age, the natural aging process can result in the weakening of pelvic muscles and connective tissues, making them more susceptible to prolapse.Hormonal Changes:
Reduced estrogen levels, particularly during menopause, can lead to changes in pelvic tissues, increasing the risk of prolapse.Chronic Straining:
Activities that involve repeated heavy lifting, chronic constipation, or conditions that cause increased abdominal pressure can contribute to the development of an enterocele.
Symptoms of enterocele may include:
A bulging sensation in the vagina.
Discomfort or pain in the pelvic region.
Problems with bowel movements, such as difficulty emptying the rectum or constipation.
Treatment options for enterocele depend on the severity of symptoms and may include:
Pelvic Floor Physical Therapy:
Exercises and techniques to strengthen the pelvic floor muscles.Lifestyle Modifications:
Maintaining a healthy weight, avoiding heavy lifting, and managing constipation can help prevent further strain on the pelvic floor.Pessaries:
Devices inserted into the vagina to support the prolapsed organs.Hormone Replacement Therapy (HRT):
Estrogen replacement therapy may be considered for postmenopausal women.Surgery:
In more severe cases or when conservative measures are ineffective, surgical intervention may be recommended to repair and support the pelvic organs.
As you can see, most of the causes and symptoms of pelvic organ prolapse are the same, it just depends on what organs are affected. If you suspect you have pelvic organ prolapse or are experiencing symptoms, come see us at Pelvic Health Center so our trained professionals can perform an examination to see if you are experiencing a prolapse and, if so, what type of prolapse is occurring. From there, we can create an accurate diagnosis and appropriate treatment plan.
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment