Back
Pudendal Neuralgia: Understanding the Causes, Symptoms, and Treatments
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 8/1/2023
Pudendal neuralgia is a term that may not be familiar to many, yet it represents a painful and potentially debilitating condition involving the pudendal nerve. Let’s delve into what pudendal neuralgia is, how it is caused, the characteristic symptoms, and how it can be treated.
What Is Pudendal Neuralgia?
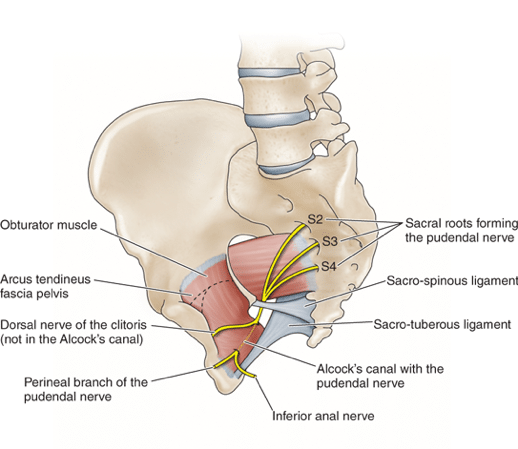
Pudendal neuralgia is primarily caused by the entrapment of the pudendal nerve, leading mostly to sensory or dermatomal deficits. It may also result in motor and autonomic deficits in some individuals. The pudendal nerve is uniquely situated between two muscles, the piriformis and coccygeus, and two pelvic structures, the sacrotuberous and sacrospinous ligaments.
Further complexity is added as the pudendal nerve splits into various branches, including the inferior rectal branch, perineal branch, and dorsal sensory nerve of the penis (in males) and clitoris (in females). This anatomical configuration is why pudendal neuralgia presents itself in various forms and may vary in signs and symptoms.
Characteristic Signs and Symptoms
Individuals with pudendal neuralgia often experience pain increased with sitting in the perineal or genital regions. Various bowel, bladder, and sexual dysfunctions may also manifest, including painful bowel movements and ejaculations. It's essential to note that the pain should not awaken an individual from sleep.
Pudendal neuralgia is classified into different types:
Type I - Entrapment below the piriformis muscle.
Type II - Entrapment between sacrospinous and sacrotuberous ligaments, the most common cause of nerve entrapment.
Type III - Entrapment in the Alcock canal.
Type IV - Entrapment of terminal branches.
Risk Factors
Certain activities and conditions may predispose individuals to pudendal neuralgia. These include biking or spinning classes, prolonged sitting, enlarged sacrospinous or sacrotuberous ligaments, chronic prostatitis, pelvic floor muscle disorders, pelvic surgery or scarring, vaginal delivery, lumbar spine stenosis, and the presence of a Tarlov Cyst.
Physical Therapy Treatment Goals and Approaches
The main objective of physical therapy when treating pudendal neuralgia is the prevention of neuropathic progression or chronicity. Treatment may involve:
Spinal Mobilization Techniques: Tailored exercises to promote spinal health.
Muscle Strengthening: Specific exercises to address muscle imbalances.
Education: Knowledge about various positioning and techniques to reduce pressure on the pudendal nerve and facilitate daily functioning.
Other non-physical therapy interventions include pudendal peripheral nerve block, an approach to providing relief through targeted nerve numbing.
Conclusion
Pudendal neuralgia is a multifaceted condition that can significantly impact an individual’s quality of life. Understanding the underlying causes, recognizing the symptoms, and seeking professional help can lead to effective treatment. Physical therapy plays a crucial role in managing this condition, offering specialized techniques and personalized care plans to alleviate pain and improve daily functioning.
If you’re experiencing pelvic floor dysfunctions including pudendal neuralgia, please reach out to us at Pelvic Health Physical Therapy Center in Madison, NJ to set up an evaluation and treatment!
Feel free to call us at 908-443-9880 or email us at contact@pelvichealthnj.com.
Resources:
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment