Back
Should I Practice My Kegels on the Toilet?
By Dr. Christine Martirez PT, DPT on 5/6/2024

A common occurrence we hear are clients telling us they practice their pelvic floor contractions, also known as Kegels, while actively urinating. While Kegels are commonly touted as a solution for pelvic floor weakness, practicing them during urination can have adverse effects on bladder function and pelvic health. Let's delve into the reasons why interrupting the natural flow of urination with Kegels can lead to problems, particularly by disrupting Bradley's loops, and explore how pelvic floor physical therapy can offer a more effective solution for addressing pelvic floor dysfunction.
Understanding Bradley's Loops and Bladder Function
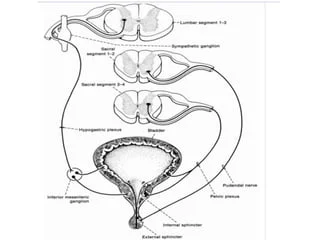
Bradley's loops refer to the intricate neural pathways that govern bladder function, including the coordination between the detrusor muscle (which contracts to expel urine) and the external urethral sphincter (which controls the release of urine). When the bladder is filling, the detrusor muscle remains relaxed, while the external urethral sphincter contracts to maintain continence. When it's time to urinate, the detrusor muscle contracts, and the external urethral sphincter relaxes, allowing urine to flow freely. There are 4 different circuits of Bradley's Loops.
Sensory Loop (Afferent Pathway):
The sensory loop, also known as the afferent pathway, involves the transmission of signals from the bladder to the brain, informing it of the bladder's status. When the bladder fills with urine, stretch receptors in the bladder wall send signals via sensory nerves (afferent fibers) to the brain, indicating the need to urinate. This loop plays a crucial role in initiating the urination process.Motor Loop (Efferent Pathway):
The motor loop, or efferent pathway, involves the transmission of signals from the brain to the bladder and pelvic floor muscles, coordinating the process of urination. When the brain receives signals indicating a full bladder, it sends messages via motor nerves (efferent fibers) to the detrusor muscle (which contracts to expel urine) and the external urethral sphincter (which relaxes to allow urine to flow). This loop ensures coordinated and controlled urination.Inhibitory Loop (Supraspinal Pathway):
The inhibitory loop, also known as the supraspinal pathway, involves higher brain centers that modulate bladder function, including the cerebral cortex and brainstem. These centers receive and interpret sensory signals from the bladder and can suppress or facilitate bladder contractions based on factors such as emotional state, cognitive function, and environmental cues. This loop provides an additional layer of control over bladder function and can influence urinary habits and behaviors.Reflex Loop (Spinal Pathway):
The reflex loop, or spinal pathway, involves reflexive responses within the spinal cord that regulate bladder function in the absence of conscious control. This loop allows for automatic coordination of bladder contractions and sphincter relaxation based on sensory input from the bladder. It plays a crucial role in maintaining continence and preventing involuntary urine leakage.
The Role of Kegels in Bladder Function
While Kegels can be beneficial for strengthening the pelvic floor muscles, practicing them during urination disrupts the natural coordination between the detrusor muscle and the external urethral sphincter. This interruption can lead to several issues:
Incomplete Emptying:
Interrupting urination with Kegels can prevent the bladder from fully emptying, leading to residual urine and increasing the risk of urinary tract infections.Urinary Urgency and Frequency:
Disrupting Bradley's loops can confuse the signals between the bladder and the brain, resulting in increased urinary urge and frequency.Overactive Bladder:
Constantly interrupting urination with Kegels can overstimulate the pelvic floor muscles, contributing to overactive bladder and urinary incontinence.
The Role of Pelvic Floor Physical Therapy
Pelvic floor physical therapy offers a holistic approach to addressing pelvic floor dysfunction and bladder issues:
Assessment:
A pelvic floor physical therapist can assess your pelvic floor function, bladder habits, and overall musculoskeletal health to identify any underlying issues contributing to urinary dysfunction.Education:
Your therapist can provide education on proper bladder habits, including the importance of relaxing the pelvic floor muscles during urination and avoiding the use of Kegels at inappropriate times.Pelvic Floor Training:
Pelvic floor physical therapy includes targeted exercises to strengthen and coordinate the pelvic floor muscles without disrupting bladder function. These exercises are tailored to your specific needs and may include relaxation techniques, biofeedback, and progressive muscle training.Behavioral Strategies:
Your therapist can teach you behavioral strategies to improve bladder control, such as bladder retraining and timed voiding techniques.Lifestyle Modifications:
Pelvic floor physical therapy may also involve recommendations for lifestyle modifications, such as dietary changes, hydration habits, and stress management techniques, to support bladder health.
While Kegels are commonly touted as a solution for pelvic floor weakness, practicing them during urination can have adverse effects on bladder function and pelvic health. By understanding the importance of Bradley's loops and seeking guidance from a pelvic floor physical therapist, you can address pelvic floor dysfunction and bladder issues effectively and safely. Pelvic floor physical therapy offers a comprehensive approach to restoring bladder function and improving pelvic health, empowering you to regain control and confidence in your bladder habits.
Looking to take control of your bladder and pelvic health? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment