Back
The Vagus Nerve and the Connection to the Pelvic Floor
By Shannon Strauch, PTA, STMT-1 on 5/10/2024
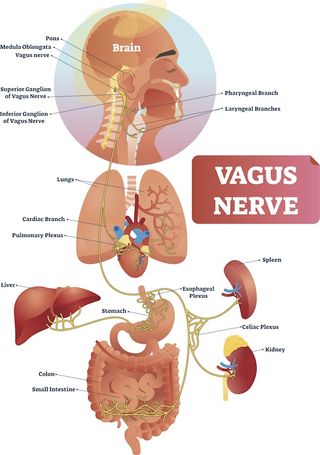
The vagus nerve, also known as the tenth cranial nerve or CN X, is a key component of the autonomic nervous system. Here's an overview of what it is, what it does, and its relationship to the pelvic floor:
1. What is the Vagus Nerve?
The vagus nerve is one of the longest and most complex nerves in the body, extending from the brainstem to various organs in the chest and abdomen.
It consists of two main branches: the sensory branch, which receives sensory information from organs like the heart, lungs, and digestive tract, and the motor branch, which controls muscles and glands in these areas.

2. Functions of the Vagus Nerve:
Parasympathetic Regulation:
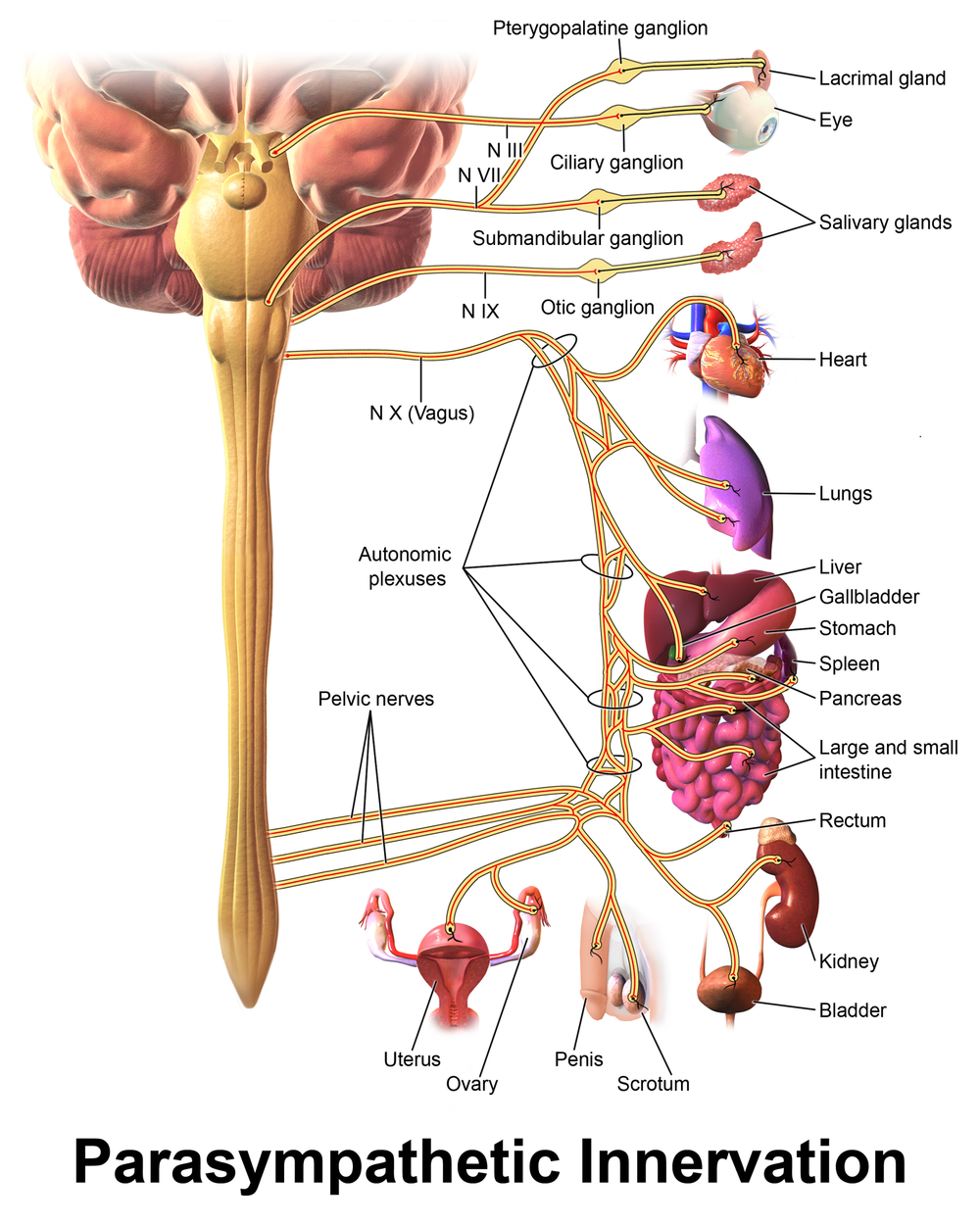
The vagus nerve plays a major role in the parasympathetic nervous system, often referred to as the "rest and digest" system. It helps regulate heart rate, breathing, and digestion, promoting relaxation and recovery.
Communication with Organs:
The vagus nerve communicates with organs such as the heart, lungs, liver, stomach, and intestines, coordinating their functions and maintaining homeostasis.
Inflammatory Response:
It also influences the body's inflammatory response, helping to reduce inflammation and promote healing.
3. Relationship to the Pelvic Floor:
Autonomic Control:
The pelvic floor is richly innervated by autonomic nerves, including branches of the vagus nerve. These nerves contribute to the regulation of pelvic floor muscle tone, bladder function, bowel movements, and sexual response.
Vagal Tone and Pelvic Health:
Optimal vagal tone, which reflects the activity and responsiveness of the vagus nerve, is associated with better pelvic floor function. It helps maintain proper coordination of pelvic floor muscles, supports bladder and bowel control, and contributes to sexual health.
Stress and Vagal Dysfunction:
Chronic stress and vagal nerve dysfunction can negatively impact pelvic floor health. Reduced vagal tone may contribute to pelvic floor disorders such as urinary incontinence, pelvic pain syndromes, and sexual dysfunction.
4. Clinical Considerations:
Healthcare providers often consider the vagus nerve's role in pelvic health when assessing and treating pelvic floor disorders.
Strategies to improve vagal tone, such as stress management techniques, diaphragmatic breathing exercises, and mindfulness practices, may complement pelvic floor therapy interventions.
In summary, the vagus nerve is a vital component of the autonomic nervous system, influencing various bodily functions including those related to the pelvic floor. Understanding its role can help in addressing pelvic floor issues and promoting overall well-being. Looking to optimize your well being with pelvic floor physical therapy? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment