Back
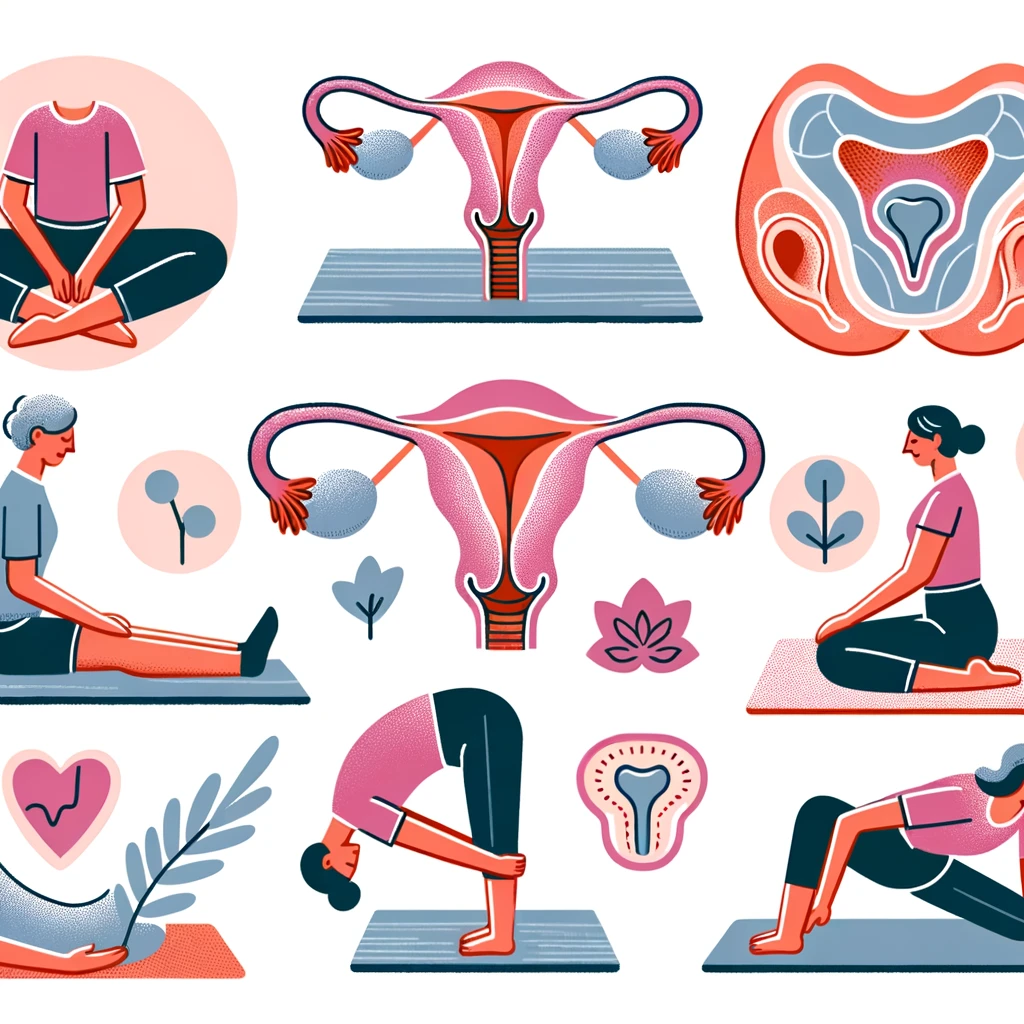
Treating Uterine Prolapse and Sciatica with Pelvic Floor Therapy
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 10/27/2023
Overview
Definition of uterine prolapse
Uterine prolapse is a condition where the uterus descends from its normal position and bulges into the vaginal canal. It is caused by weakened pelvic floor muscles and ligaments that support the uterus.
Definition of sciatica
Sciatica is a type of nerve pain that radiates from the lower back down to the legs. It is caused by compression or irritation of the sciatic nerve, which is the longest nerve in the body.
Connection between uterine prolapse and sciatica
Uterine prolapse can cause sciatica due to the pressure and strain it puts on the pelvic floor muscles and nerves. As the uterus descends, it can compress the sciatic nerve, leading to pain, numbness, and tingling sensations in the lower back and legs.
Importance of pelvic floor therapy in treating uterine prolapse and sciatica
Pelvic floor therapy is a non-invasive treatment that focuses on strengthening and retraining the pelvic floor muscles. It can help alleviate symptoms of both uterine prolapse and sciatica by improving muscle strength and function, reducing pressure on the nerves, and promoting proper alignment of the pelvic organs.
Additionally, pelvic floor therapy can also address any underlying issues that may contribute to uterine prolapse and sciatica, such as poor posture, weak core muscles, and hormonal imbalances.
It is important to seek professional guidance from a pelvic floor therapist to ensure proper techniques and exercises are being performed to effectively treat uterine prolapse and sciatica.
Understanding Uterine Prolapse
Causes of Uterine Prolapse
Uterine prolapse occurs when the muscles and ligaments that support the uterus weaken, causing the uterus to descend into the vaginal canal. This weakening can be caused by a variety of factors, including:
Pregnancy and childbirth, which can stretch and weaken the pelvic floor muscles
Aging, as the muscles and ligaments naturally weaken over time
Chronic constipation or straining during bowel movements
Obesity, which puts extra pressure on the pelvic floor muscles
Repeated heavy lifting or strenuous physical activity
Symptoms of Uterine Prolapse
The symptoms of uterine prolapse can vary depending on the severity of the condition, but may include:
A feeling of pressure or fullness in the pelvic area
A sensation of something bulging or protruding from the vagina
Difficulty emptying the bladder or bowels
Pain or discomfort during sexual intercourse
Lower back pain
Risk Factors for Uterine Prolapse
While any woman can develop uterine prolapse, there are certain factors that may increase the risk, including:
Multiple pregnancies and vaginal deliveries
Being over the age of 50
Having a family history of uterine prolapse
Being overweight or obese
Having a job or lifestyle that involves heavy lifting or straining
Diagnosis of Uterine Prolapse
If you are experiencing symptoms of uterine prolapse, your pelvic floor physical therapist (PFPT) will perform a physical exam to check for any signs of prolapse. This may include a pelvic exam, where your PFPT will visually inspect the vagina and cervix, as well as a pelvic floor muscle strength test. In some cases, imaging tests such as an ultrasound or MRI may be ordered to get a better view of the pelvic organs and their position.
Understanding Sciatica
Causes of Sciatica
Sciatica is a condition that occurs when the sciatic nerve, which runs from the lower back down through the hips and buttocks and into the legs, becomes compressed or irritated. This compression or irritation can be caused by a variety of factors, including:
Herniated or bulging discs in the spine
Spinal stenosis (narrowing of the spinal canal)
Degenerative disc disease
Spinal injuries or trauma
Pregnancy and childbirth
Obesity
Symptoms of Sciatica
The most common symptom of sciatica is pain that radiates from the lower back down through the buttocks and into one or both legs. This pain can range from mild to severe and may be accompanied by other symptoms such as:
Numbness or tingling in the affected leg
Muscle weakness in the affected leg
Burning or shooting pain down the leg
Difficulty standing or walking
Risk Factors for Sciatica
While anyone can develop sciatica, there are certain factors that may increase your risk, including:
Age (sciatica is more common in people over 40)
Occupations that involve heavy lifting or prolonged sitting
Obesity
Diabetes
Sedentary lifestyle
Previous spinal injuries or conditions
Diagnosis of Sciatica
If you are experiencing symptoms of sciatica, your doctor will likely perform a physical exam and may order imaging tests such as X-rays, MRI, or CT scan to confirm the diagnosis. They may also conduct nerve conduction studies to determine the extent of nerve damage.
Connection between Uterine Prolapse and Sciatica
How uterine prolapse can cause sciatica
Uterine prolapse occurs when the muscles and ligaments that support the uterus weaken, causing the uterus to descend into the vaginal canal. This can put pressure on the nerves in the pelvic area, including the sciatic nerve. As a result, the sciatic nerve can become compressed or irritated, leading to sciatica symptoms such as pain, numbness, and tingling in the lower back, buttocks, and legs.
How sciatica can be a symptom of uterine prolapse
Sciatica is a common symptom of uterine prolapse, as the two conditions are closely connected. The pressure on the sciatic nerve caused by the prolapsed uterus can lead to sciatica symptoms. However, it is important to note that not all cases of sciatica are caused by uterine prolapse, and other underlying conditions should be ruled out by a healthcare professional.
Importance of addressing both conditions simultaneously
It is crucial to address both uterine prolapse and sciatica simultaneously if you are experiencing both, as treating one condition without addressing the other can lead to incomplete relief of symptoms. For example, if only the sciatica is treated, the underlying cause of uterine prolapse may worsen, leading to a recurrence of sciatica symptoms. Therefore, a comprehensive treatment plan that addresses both conditions is necessary for long-term relief.
Potential complications of untreated uterine prolapse and sciatica
If left untreated, uterine prolapse and sciatica can lead to various complications. Untreated uterine prolapse can cause discomfort, difficulty with bowel movements and urination, and sexual dysfunction. Sciatica, if left untreated, can lead to chronic pain and disability, affecting daily activities and quality of life. It is essential to seek treatment for both conditions to prevent these potential complications.
Role of Pelvic Floor Therapy in Treating Uterine Prolapse and Sciatica
What is Pelvic Floor Therapy?
Pelvic floor therapy is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues in the pelvic region. These muscles play a crucial role in supporting the pelvic organs, including the uterus, bladder, and rectum. Pelvic floor therapy involves exercises, stretches, and other techniques to strengthen and improve the function of these muscles.
How Pelvic Floor Therapy Can Help with Uterine Prolapse
Uterine prolapse occurs when the muscles and ligaments that support the uterus become weak or damaged, causing the uterus to descend into the vaginal canal. This can lead to discomfort, urinary incontinence, and other symptoms. Pelvic floor therapy can help by strengthening the pelvic floor muscles, which in turn can provide better support for the uterus and prevent further descent. It can also improve bladder control and reduce symptoms of prolapse.
How Pelvic Floor Therapy Can Help with Sciatica
Sciatica is a condition that occurs when the sciatic nerve, which runs from the lower back down the legs, becomes compressed or irritated. This can cause pain, numbness, and tingling in the lower back, buttocks, and legs. Pelvic floor therapy can help with sciatica by addressing any underlying pelvic floor dysfunction that may be contributing to the compression of the sciatic nerve. By improving pelvic floor muscle strength and function, it can alleviate pressure on the nerve and reduce symptoms of sciatica.
Benefits of Pelvic Floor Therapy for Overall Pelvic Health
Pelvic floor therapy not only helps with specific conditions like uterine prolapse and sciatica, but it also has numerous benefits for overall pelvic health. By strengthening the pelvic floor muscles, it can improve bladder and bowel control, reduce pelvic pain, and enhance sexual function. It can also help prevent future pelvic floor issues and improve overall quality of life.
Pelvic Floor Therapy Exercises for Uterine Prolapse and Sciatica
Kegel Exercises for Strengthening Pelvic Floor Muscles
Kegel exercises are a type of pelvic floor exercise that involve contracting and relaxing the muscles of the pelvic floor. These exercises can help strengthen the muscles that support the uterus and prevent it from prolapsing. They can also improve sciatica symptoms by increasing blood flow and reducing tension in the pelvic area.
Pelvic Tilts for Improving Pelvic Alignment
Pelvic tilts involve tilting the pelvis forward and backward while lying on your back. This exercise can help improve pelvic alignment and reduce strain on the pelvic floor muscles. It can also alleviate sciatica pain by relieving pressure on the sciatic nerve.
Bridge Pose for Strengthening Glute Muscles
Bridge pose is a yoga pose that involves lifting the hips off the ground while lying on your back. This exercise can help strengthen the glute muscles, which play a role in supporting the pelvic floor. Strong glutes can help prevent uterine prolapse and improve sciatica symptoms.
Pelvic Floor Stretches for Relieving Tension and Pain
In addition to exercises that strengthen the pelvic floor muscles, it's important to also stretch these muscles to relieve tension and pain. A pelvic floor therapist can recommend specific stretches based on your individual needs and symptoms. Some common stretches include butterfly stretch, child's pose, and deep squats.
Other Exercises Recommended by a Pelvic Floor Therapist
In addition to the exercises mentioned above, a pelvic floor therapist may recommend other exercises to help with uterine prolapse and sciatica. These may include pelvic floor releases, pelvic floor massage, and core strengthening exercises. It's important to work with a therapist to develop a personalized exercise plan that addresses your specific needs and goals.
If you are experiencing pelvic floor dysfunctions associated with the issues above, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment