Back
What is Gastroparesis and How Can A Pelvic Floor Physical Therapist Help Me?
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 10/6/2023
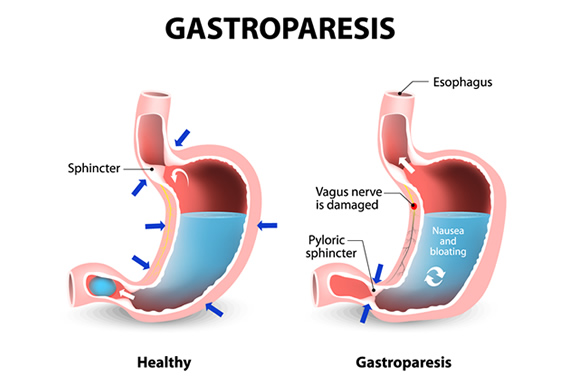
Gastroparesis is a condition that affects the digestive system, specifically the stomach. It is a disorder where the muscles in the stomach are unable to properly contract and push food through the digestive tract. This causes food to remain in the stomach for a longer period of time, leading to uncomfortable symptoms such as nausea, bloating, and vomiting. Gastroparesis can be caused by various factors such as diabetes, nerve damage, and certain medications. Pelvic floor physical therapy (PFPT) is a specialized form of physical therapy that focuses on the pelvic floor muscles. These muscles play a crucial role in supporting the organs in the pelvic region, including the bladder, uterus, and the bowels. They also play a role in controlling bowel and bladder movements. When these muscles are dysfunctional or weak, it can lead to a range of health issues, including digestive problems such as gastroparesis. The purpose of this article is to explore the connection between gastroparesis and pelvic floor physical therapy. While gastroparesis is typically treated with medications and dietary changes, PFPT has emerged as a potential treatment option for managing the symptoms and improving the quality of life for individuals with this condition. This article aims to provide an in-depth understanding of how this specialized form of physical therapy can help treat gastroparesis and improve digestive health. In recent years, the use of PFPT for managing gastroparesis has gained attention, and many healthcare professionals have recommended this approach to their patients.
The pelvic floor muscles are closely connected to the digestive system, and studies have shown that dysfunction in these muscles can contribute to the development or worsening of gastroparesis symptoms. By addressing these underlying muscle issues, PFPT can help alleviate the symptoms of gastroparesis and improve the overall functioning of the digestive system. One of the key techniques used in PFPT for gastroparesis is biofeedback. This involves using specialized equipment to monitor the activity of the pelvic floor muscles and provide visual feedback to the patient. This helps the patient become more aware of their pelvic floor muscles and learn how to properly engage and relax them. Biofeedback has been shown to be effective in improving symptoms of gastroparesis, such as nausea and bloating, as well as in reducing the time it takes for food to empty from the stomach.
In addition to biofeedback, PFPT also utilizes exercises to help strengthen and improve the function of the pelvic floor muscles. These exercises, known as pelvic floor muscle training, involve performing specific movements and contractions to target the muscles in the pelvic region. This can help improve the coordination and control of these muscles, leading to better digestion and symptom management for individuals with gastroparesis. Pelvic Floor Therapists are also trained in what is called Visceral Mobilizations, which are manual techniques used to help internal organs operate more efficiently. In conclusion, PFPT is a valuable treatment option for individuals with gastroparesis. By addressing the underlying issues in the pelvic floor muscles, this specialized form of physical therapy can help improve symptoms and overall digestive health. As always, it is important to consult with a healthcare professional to determine the best treatment plan for your specific condition.
Understanding Gastroparesis
A. Definition and Symptoms
Gastroparesis is a chronic digestive disorder that affects the movement of food from the stomach to the small intestine. It occurs when the nerves and muscles in the stomach are damaged or weakened, leading to delayed or incomplete emptying of the stomach. Common symptoms of gastroparesis include nausea, vomiting, bloating, early satiety, and abdominal pain. These symptoms can vary in severity and frequency and can greatly affect an individual’s quality of life.
B. Causes and Risk Factors
Gastroparesis can have various underlying causes, including diabetes, nerve damage, connective tissue disorders, and certain medications. In diabetic individuals, high blood sugar levels can damage the nerves that control stomach function, resulting in gastroparesis. Other risk factors for gastroparesis include abdominal surgery, viral infections, hypothyroidism, and eating disorders.
C. Diagnosis and Treatment Options
Gastroparesis is often misdiagnosed or undiagnosed because its symptoms can overlap with other digestive disorders. To properly diagnose gastroparesis, your doctor may perform a physical exam, review your medical history, and recommend tests such as gastric emptying scintigraphy, gastric manometry, and breath tests. Once diagnosed, treatment for gastroparesis aims to relieve symptoms and improve stomach emptying. One effective treatment for gastroparesis is pelvic floor physical therapy (PFPT). This type of therapy focuses on the muscles and nerves in the pelvic floor, which are essential for proper digestion and bowel function.
Here’s how PFPT can help treat gastroparesis:
1. Improved Pelvic Floor Muscle Function The pelvic floor muscles play a vital role in the digestive process by aiding in the relaxation and contraction of the stomach and intestines. If these muscles are weak or poorly coordinated, it can lead to delayed gastric emptying and other gastrointestinal issues. By performing targeted exercises and techniques, PFPT can strengthen and improve the coordination of the pelvic floor muscles, resulting in better digestion.
2. Increased Abdominal Muscle Strength The abdominal muscles also play a significant role in digestion by supporting the organs and assisting in the emptying of the stomach. Poor abdominal muscle strength can lead to abdominal bloating, discomfort, and delayed gastric emptying. PFPT can help to strengthen these muscles, which can improve overall digestion and reduce symptoms of gastroparesis.
3. Relief of Pelvic Floor Dysfunction Symptoms Many individuals with gastroparesis also experience symptoms related to pelvic floor dysfunction, such as constipation, urinary incontinence, or pelvic pain. These symptoms can further complicate the management of gastroparesis. By addressing pelvic floor dysfunction through PFPT, these symptoms can be reduced, making it easier to manage gastroparesis. In conclusion, gastroparesis is a chronic digestive disorder that can greatly impact an individual’s quality of life. It is crucial to understand the definition, symptoms, causes, and risk factors of this condition. For those with gastroparesis, pelvic floor physical therapy offers an effective and targeted approach to improve symptoms and promote healthy digestion. Consult with a healthcare professional to determine if PFPT is a suitable treatment option for your gastroparesis. ---
Role of Pelvic Floor Physical Therapy
A. Explanation of Pelvic Floor Muscles The pelvic floor muscles play a crucial role in the functioning of our digestive system. These muscles are a group of muscles that form a hammock-like structure at the bottom of the pelvis, supporting the pelvic organs such as the bladder, uterus, and rectum. They also help to control the opening and closing of the anus and the urethra. When these muscles are weak or dysfunctional, it can lead to issues like incontinence, constipation, and even gastroparesis.
B. Connection between Gastroparesis and Pelvic Floor Dysfunction Gastroparesis is a condition where the stomach takes longer than normal to empty its contents into the small intestine. This delay in gastric emptying can be caused by various factors, including pelvic floor dysfunction. When the pelvic floor muscles are not functioning properly, it can result in poor coordination between the stomach and the small intestine, leading to gastroparesis. Additionally, constipation, which is a common symptom of pelvic floor dysfunction, can also contribute to the development of gastroparesis.
C. Benefits of Physical Therapy for Gastroparesis Pelvic floor physical therapy can be an effective treatment option for managing gastroparesis. The goal of this therapy is to improve the strength, coordination, and flexibility of the pelvic floor muscles, which can help alleviate symptoms and improve gastric emptying. Here are some of the key benefits of physical therapy for gastroparesis:
1. Improved Muscle Function: Through targeted exercises and techniques, physical therapy can help to strengthen and relax the pelvic floor muscles, improving their overall function. This can help to promote better coordination between the stomach and the small intestine, leading to more efficient gastric emptying.
2. Relief from Constipation: One of the common symptoms of pelvic floor dysfunction is constipation. By addressing the root cause of this issue, physical therapy can help to improve bowel movements and alleviate constipation. This, in turn, can reduce the pressure on the stomach and improve gastric emptying.
3. Education and Lifestyle Modifications: In addition to exercises, physical therapy also involves educating patients about their condition and making necessary lifestyle modifications, such as dietary changes, to manage gastroparesis symptoms. This holistic approach can greatly enhance the effectiveness of treatment.
4. Non-Invasive and Non-Medicated Treatment: Physical therapy for gastroparesis is a non-invasive and non-medicated treatment option, making it a safe and natural choice for those seeking relief from their symptoms. It also has no side effects, making it suitable for long-term use. In conclusion, pelvic floor physical therapy can play a vital role in managing gastroparesis. By addressing pelvic floor dysfunction, this therapy can help to improve muscle function, relieve constipation, and promote more efficient gastric emptying. If you are struggling with gastroparesis, talk to a pelvic floor physical therapist to learn more about how this treatment can help you.
Steps to Treat Gastroparesis with Pelvic Floor Physical Therapy
When it comes to treating gastroparesis with pelvic floor physical therapy, there are several key steps that are essential for a successful outcome. These steps involve thorough assessment and evaluation, developing a tailored treatment plan, determining the frequency and duration of therapy, and making adjustments and modifications as needed. Let's take a closer look at each of these steps in detail.
Assessment and Evaluation
The first step in treating gastroparesis with pelvic floor physical therapy is to thoroughly assess and evaluate the patient. This involves understanding the patient's symptoms, assessing their pelvic floor muscle strength, and identifying any trigger points and muscle tension in the pelvic floor muscles. Understanding the patient's symptoms is crucial in determining the best course of treatment. Gastroparesis is a condition that results in delayed gastric emptying, causing symptoms such as abdominal pain, nausea, bloating, and early satiety. However, in addition to these typical symptoms, some patients may also experience pelvic pain and dysfunction, which is where pelvic floor physical therapy comes into play. It is important for the therapist to understand the patient's specific symptoms and how they are affecting their daily life. Assessing the pelvic floor muscle strength is also a critical aspect of the evaluation process. Weak pelvic floor muscles can contribute to gastroparesis by causing decreased pelvic organ support and impairing normal intestinal motility. On the other hand, overly tense pelvic floor muscles can also contribute to gastroparesis symptoms by causing excessive tension and compression on the pelvic organs and nerves. Therefore, it is crucial for the therapist to assess the strength and tension of the pelvic floor muscles to determine the root cause of the patient's symptoms. Trigger points are areas of muscle tension and tenderness that can cause referred pain and discomfort. These trigger points can be present in the pelvic floor muscles and can contribute to gastroparesis symptoms. A thorough assessment and evaluation by a trained pelvic floor physical therapist will help identify any trigger points in the pelvic floor muscles that may need to be addressed as part of the treatment plan.
Tailored Treatment Plan
Once the patient's symptoms, muscle strength, and trigger points have been assessed and evaluated, the next step is to develop a tailored treatment plan. This plan will be specific to each individual patient, taking into account their unique symptoms and needs. Targeting specific muscles is an important aspect of treatment for gastroparesis with pelvic floor physical therapy. This may involve using techniques such as manual therapy, where the therapist uses their hands to apply pressure and release any areas of muscle tension and trigger points. Biofeedback is another technique that can be used to help the patient become more aware of their pelvic floor muscles and learn how to relax them. Breathing exercises can also be incorporated to help release tension in the pelvic floor muscles and improve overall muscle function. In addition to targeted muscle techniques, lifestyle and dietary changes may also be recommended by the therapist. Specific dietary modifications, such as eating smaller, more frequent meals, avoiding foods that aggravate gastroparesis symptoms, and increasing fluid intake, may be recommended. The therapist may also advise the patient to avoid or modify certain activities that can contribute to pelvic floor muscle tension, such as heavy lifting or prolonged sitting.
Frequency and Duration of Therapy
The frequency and duration of therapy will vary depending on the severity of the patient's symptoms and their response to treatment. In general, it is recommended to attend pelvic floor physical therapy sessions 1-2 times per week. This allows for consistent progress to be made while also giving the patient time to practice techniques and exercises at home. The timeline for improvement may also vary from patient to patient. Some individuals may experience relief from their symptoms within a few weeks of starting therapy, while others may take longer. It is important for patients to be patient and consistent with their treatment plan to achieve the best results.
Adjustments and Modifications
As with any form of therapy, adjustments and modifications may need to be made along the way. It is important for the therapist to monitor the patient's progress and make any necessary changes to the treatment plan. This may involve adding or changing exercises, modifying the frequency or duration of therapy, or addressing any setbacks or difficulties that the patient may be experiencing. In conclusion, treating gastroparesis with pelvic floor physical therapy involves a thorough assessment and evaluation, developing a tailored treatment plan, determining the frequency and duration of therapy, and making adjustments and modifications as needed. With a dedicated and knowledgeable therapist and a commitment to consistent therapy, patients with gastroparesis can find relief from their symptoms and improve their overall quality of life. ---
Additional Resources and Tips
A. Recommended Dietary Changes for Gastroparesis Making dietary changes is an important aspect of treating gastroparesis with pelvic floor physical therapy. The goal is to ease the workload of the digestive system by consuming foods that are easier to digest. This can help reduce symptoms such as bloating, nausea, and abdominal pain. A registered dietitian can help create a personalized meal plan based on your specific needs and preferences. Here are some general recommendations to follow:
- Eat smaller, more frequent meals: This can help ease the burden on the digestive system and reduce symptoms.
- Choose low-fat foods: High-fat foods can slow down digestion and worsen symptoms. Aim for lean protein sources and limit fried foods.
- Opt for soft or pureed foods: These are easier to digest and put less strain on the digestive system.
- Avoid high-fiber foods: Fiber can be difficult for the digestive system to break down, so it's best to limit foods such as whole grains, raw vegetables, and fruits with skins or seeds.
- Stay hydrated: Drinking plenty of water throughout the day can help keep your stomach and intestines moving and prevent constipation.
- Keep a food diary: Tracking your food intake and symptoms can help identify trigger foods and make necessary adjustments to your diet.
B. Other Helpful Exercises and Techniques In addition to pelvic floor physical therapy, there are other exercises and techniques that can help manage symptoms of gastroparesis and pelvic floor dysfunction. These include:
- Diaphragmatic breathing: Slow, deep breathing exercises can help relax the abdominal muscles and improve digestion.
- Gentle abdominal massage: This can help stimulate bowel movement and relieve abdominal discomfort.
- Relaxation techniques: Stress and anxiety can worsen symptoms of gastroparesis and pelvic floor dysfunction. Practicing relaxation techniques such as meditation, yoga, or tai chi can help reduce stress and promote better digestive function.
C. Support Groups and Online Resources for Gastroparesis and Pelvic Floor Dysfunction Living with gastroparesis and pelvic floor dysfunction can be challenging, both physically and emotionally. Connecting with others who are going through a similar experience can provide valuable support and information. Consider joining a support group or participating in online forums to connect with other individuals and learn from their experiences. Additionally, there are several reputable online resources available, including websites, blogs, and social media pages, that provide information, community support, and updates on the latest treatment options for gastroparesis and pelvic floor dysfunction.
D. Importance of Communication with Healthcare Team Lastly, communication with your healthcare team is crucial for successfully managing gastroparesis and pelvic floor dysfunction. Be sure to regularly follow-up with your doctor and physical therapist to discuss your progress and address any concerns or difficulties you may be experiencing. It's essential to inform your healthcare team about any changes in symptoms, as they can provide guidance and make necessary adjustments to your treatment plan. Open and honest communication with your healthcare providers can help ensure that you receive the best care and support for your condition. ---
Conclusion
In this article, we have thoroughly discussed the use of pelvic floor physical therapy in the treatment of gastroparesis. Gastroparesis is a condition characterized by delayed stomach emptying and can cause uncomfortable digestive symptoms such as nausea, vomiting, and bloating. While traditional treatment methods such as medication and dietary changes can be helpful, pelvic floor physical therapy has emerged as a promising option for managing gastroparesis symptoms. During pelvic floor physical therapy, a trained therapist will work with the muscles and tissues in the pelvic floor to address any dysfunctions that may be contributing to gastroparesis symptoms. This may include muscle tension, weakness, or coordination issues. By targeting the muscles in the pelvic floor, which play a crucial role in digestive function, pelvic floor physical therapy can improve the symptoms and overall quality of life for those living with gastroparesis.
Due to the complex nature of gastroparesis and the unique needs of each individual's body, it is crucial to seek professional help when considering pelvic floor physical therapy as a treatment option. A trained physical therapist specializing in pelvic floor disorders will have the knowledge and skills to properly assess and treat the specific pelvic floor dysfunctions contributing to gastroparesis. They can also provide personalized exercises and techniques tailored to each patient's needs, ensuring the best chance for improvement. Additionally, seeking professional help can help avoid potential risks or exacerbation of symptoms. Without proper training and guidance, attempting pelvic floor physical therapy on your own can cause more harm than good. It is essential to work with a professional who can monitor progress and adjust treatment as needed to ensure optimal results.
Finally, we would like to emphasize the importance of ongoing treatment and management of gastroparesis with pelvic floor physical therapy. While initial treatment may bring relief from symptoms, continuing to work with a therapist on a regular basis can help maintain progress and prevent a recurrence of symptoms. Additionally, incorporating exercises and techniques into daily routines can help manage gastroparesis in the long term. In conclusion, pelvic floor physical therapy has shown great potential in the treatment of gastroparesis. By addressing underlying pelvic floor dysfunctions, this therapy can provide relief from uncomfortable digestive symptoms and improve overall quality of life. However, it is crucial to seek professional help and commit to ongoing treatment and management for the most effective results.
Read More:
How Visceral Mobilization Can Assist with the Treatment of SIBO By Dr. Christine Martirez PT, DPT on 10/22/2024 Learn about SIBO and how visceral mobilizations can be an integral part of your recovery journey Understanding Sacral Pain and How Pelvic Floor Therapy Can Help By Dr. Christine Martirez PT, DPT on 10/21/2024 Learn about sacral pain & how pelvic floor therapy can be an intregral part of your healing journey
Are you ready to live pain free?
Request An Appointment