Back
What is Prostatitis and how can PFPT help me?
By Dr. Zarina Vitebsky, DPT, MSPT, PRPC, TPS, LPF, DN on 1/29/2023

Prostatitis is a disorder of the prostate gland typically associated with inflammation. It often causes painful or difficult urination, as well as pain in the groin, pelvic area, and/or genitals. Additionally, the patient may experience pain with urination, erection and ejaculation, and even sitting or standing. Bacterial infections are responsible for many (but not all) episodes of prostatitis.
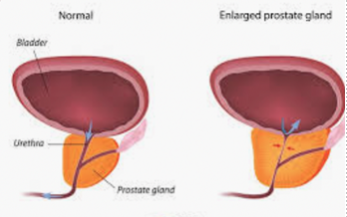
The prostate gland, which is about the size of a walnut when healthy, is located just below the urinary bladder in men. It surrounds the top portion of the urethra - the tube which drains urine from the bladder. The prostate gland, along with other sex glands in the pelvis, produces the fluid (semen) that transports sperm during ejaculation.
There are generally four types of prostatitis:
Acute Bacterial Prostatitis
occurs with a bacterial infection of the prostate gland and usually appears with sudden, severe symptoms.Chronic Bacterial Prostatitis
occurs when there is a persistent or recurring bacterial infection. Unlike acute bacterial prostatitis, symptoms are less severe; however, they do occur over a longer period of time.Chronic Prostatitis,
or Chronic Pelvic Pain Syndrome as it is also known, is identified by ongoing or recurrent pelvic pain and urinary tract symptoms without any evidence of infection.Asymptomatic Inflammatory Prostatitis
presents with an inflamed prostate gland without the appearance of the typical symptoms.
What are the symptoms of prostatitis?
Signs and symptoms of prostatitis can vary depending on the type of prostatitis you are experiencing. Some of the more common symptoms include:
Pain or burning sensation when urinating (dysuria),
Difficulty urinating, such as difficulty starting a stream or dribbling,
Frequent urination, particularly at night (nocturia),
Urinary urgency,
Pain in the abdomen, groin, and/or lower back,
Perineal pain (in the area between the scrotum and rectum),
Pain or discomfort in the penis or testicles,
Painful erection and/or ejaculation.
How can Pelvic Floor Physical Therapy help me?
According to the latest research, techniques applied to the pelvic floor both externally and internally, when performed by a certified pelvic floor physical therapist, appeared to be beneficial to patients in reducing pain and improving overall sexual function.1
When you schedule an appointment for Pelvic Floor Physical Therapy, your first visit will be a detailed evaluation of all necessary subjective (how you feel and experience symptoms) and objective (any labs or imaging that may have been performed prior to your visit, along with physical examination by your Pelvic Floor Physical Therapist) information that will determine the root cause and contributing factors to each of the patient's concerns. By the end of this conversation and examination, the Physical Therapist will discuss their findings with the patient, work with the patient to develop a customized plan of care addressing target areas, and create a home exercise program to complement the treatments the patient will receive during regular office therapy sessions. Together, therapist and patient will work towards restoring optimal functioning.
Some common therapeutic techniques used in the treatment of prostatitis include:
Coordination exercises and training,
Therapeutic exercise,
Manual therapy such as myofascial release, soft tissue mobilization, trigger point release, joint mobilization, and ligament release,
Relaxation exercises,
Diaphragmatic breathing,
Postural education and training,
Behavioral recommendations modifying neuroplasticity,
Other modalities such as e-stim, TENS, ultrasound, etc.,
and, of course, the Home Exercise Plan.
------------------------------
1(Physical Therapist Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome, Linda S. Van Alstyne,Kendra L. Harrington,Esther M. Haskvitz, Physical Therapy, Volume 90, Issue 12, 1 December 2010, Pages 1795–1806).
Read More:
Dry Needling for C-Section Scars and Postpartum Recovery By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn how dry needling can be used for c-section scars and c-section recovery How Red Light Therapy Can Be Used to Treat Pelvic Floor Dysfunctions By Dr. Christine Martirez PT, DPT on 10/15/2024 Learn about red light therapy and how it can be used to treat pelvic floor dysfunctions
Are you ready to live pain free?
Request An Appointment