Back
Why do I have Pelvic Organ Prolapse after Childbirth?
By Shannon Strauch, PTA, STMT-1 on 7/2/2024
Pelvic organ prolapse (POP) occurs when the muscles and tissues supporting the pelvic organs (such as the bladder, uterus, rectum, or intestines) become weakened or stretched, causing one or more of these organs to drop or press into or out of the vaginal canal. This condition can affect women of all ages but is more common after childbirth, menopause, or pelvic surgery.
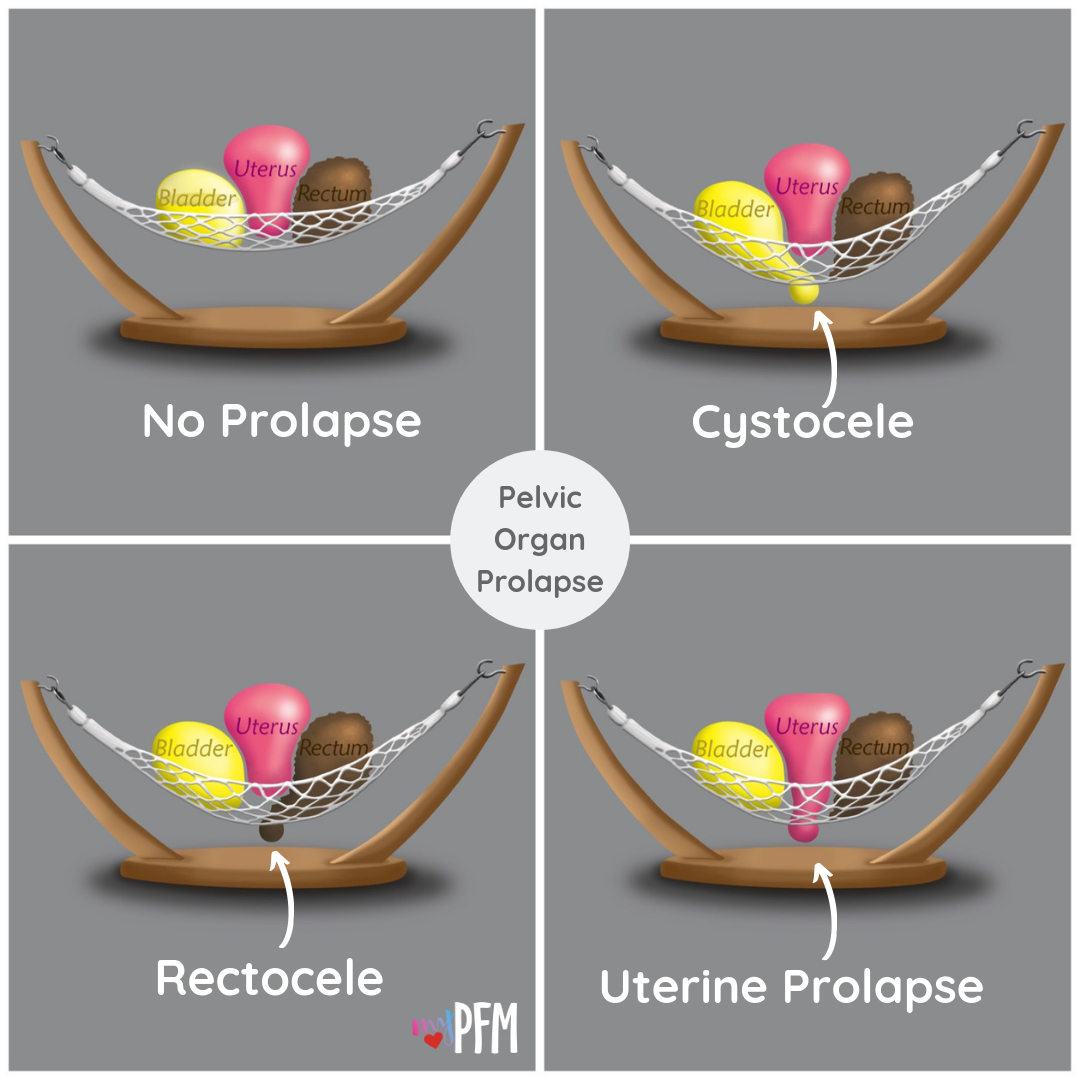
There are different types of pelvic organ prolapse, each named according to the organ that is affected:
Cystocele (Anterior Prolapse):
This occurs when the bladder drops into the front wall of the vagina.Rectocele (Posterior Prolapse):
This happens when the rectum bulges into the back wall of the vagina.Uterine Prolapse:
This is when the uterus descends into the vaginal canal.Enterocele:
This involves the small intestine pushing against the vaginal wall, usually occurring in women who have had a hysterectomy.Vaginal Vault Prolapse:
This occurs when the top of the vaginal canal drops, which can happen after a hysterectomy.
Symptoms of Pelvic Organ Prolapse
The symptoms of POP can vary depending on the severity and the specific organs involved but often include:
A feeling of pressure or fullness in the pelvic area
A visible bulge or protrusion from the vaginal opening
Pelvic pain or discomfort
Lower back pain
Urinary problems, such as incontinence, urgency, or difficulty emptying the bladder
Bowel problems, such as constipation or difficulty with bowel movements
Pain during sexual intercourse
Pregnancy and Prolapse
Prolapse after pregnancy can occur due to various reasons:
Weakened Pelvic Floor Muscles:
During pregnancy and childbirth, the pelvic floor muscles can become stretched and weakened, leading to decreased support for the pelvic organs.Hormonal Changes:
Fluctuations in hormone levels during pregnancy and postpartum can affect the strength and tone of the pelvic floor muscles and connective tissues.Childbirth Trauma:
Vaginal childbirth, especially if it's prolonged or involves instruments like forceps, can increase the risk of pelvic organ prolapse by damaging supportive tissues.Increased Abdominal Pressure:
Factors such as carrying multiples, excessive weight gain during pregnancy, chronic constipation, or heavy lifting postpartum can increase intra-abdominal pressure, straining the pelvic floor.Genetic Predisposition:
Some individuals may have a genetic predisposition to weaker connective tissues, making them more susceptible to pelvic organ prolapse.
Pelvic Floor Therapy and Prolapse
Pelvic floor therapy (or physical therapy) can help in several ways:
Muscle Strengthening:
Therapists can prescribe exercises to specifically target and strengthen the pelvic floor muscles, improving their ability to support pelvic organs and reduce prolapse symptoms.Education:
Patients can learn proper techniques for pelvic floor muscle activation and relaxation, which can prevent further strain and support better pelvic floor function.Behavioral Changes:
Therapists can provide guidance on lifestyle modifications, such as proper lifting techniques, managing constipation, and maintaining a healthy weight, to reduce intra-abdominal pressure on the pelvic floor.Manual Therapy:
Techniques such as myofascial release or manual therapy can help release tight muscles and improve pelvic floor mobility and function.Biofeedback:
These techniques can help patients better understand and strengthen their pelvic floor muscles by providing real-time feedback and enhancing muscle recruitment.
Overall, pelvic floor therapy is personalized to address the specific needs of individuals experiencing pelvic organ prolapse after pregnancy, focusing on strengthening, support, and lifestyle adjustments to improve pelvic floor health and function. Experiencing pelvic organ prolapse after childbirth? Reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com.
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment