Back
Why Is There A Ton Of Pressure in My Rectum?: Comprehensive Guide to Male Pelvic Floor Dysfunctions
By Pelvic Health Physical Therapy on 2/2/2024
Men (or those with male genitals)! Have you ever had to put the following in the Google Search Engine: “golf ball in butthole/rectum feeling,” “there’s a ton of pressure in my rectum,” “there’s something stuck in my rectum,” “my tailbone hurts every time I sit,” “I can’t drive for long periods of time.” If this sounds like you, you may be experiencing one of the following diagnoses below.
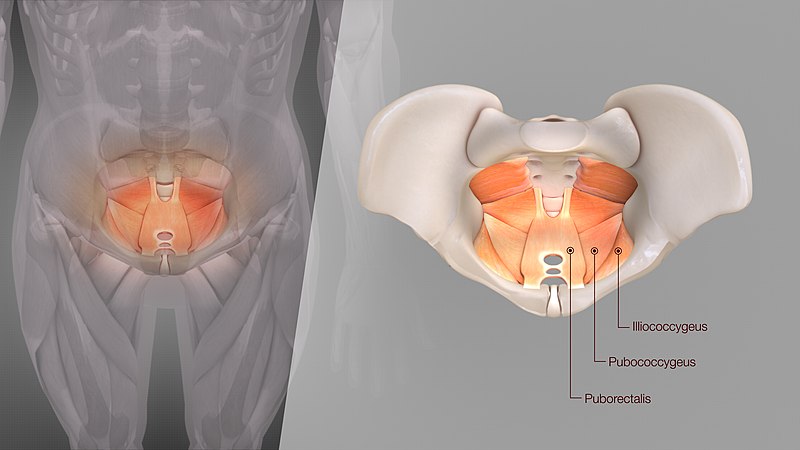
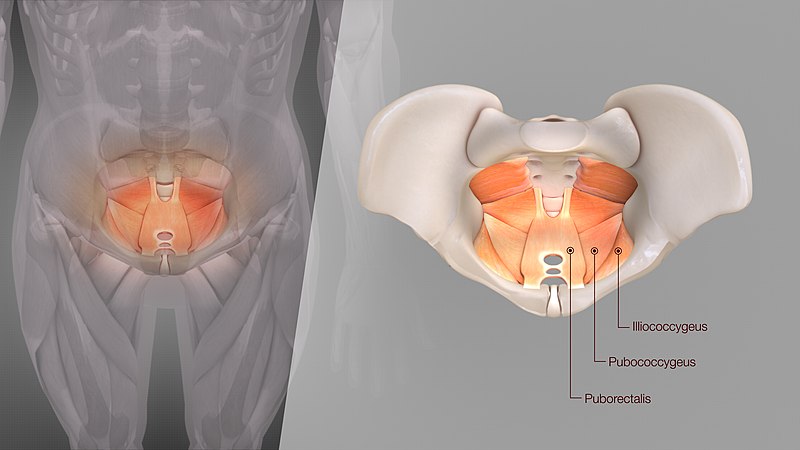
Levator Ani Syndrome
Your levator ani muscles consist of a group of muscles in your pelvic floor that help support pelvic organs. Their primary function is to elevate the pelvic floor. Levator ani syndrome is a spasm of those muscles causing symptoms of tailbone pain, ball in rectum feeling, and/or feelings of UTI. Levator ani syndrome can be caused by:
Orthopedic conditions: such as hip trauma, lower back issues, fall on tailbone, and/or surgery in and around the area, causing them to spasm.
Stress: the levator ani (and the pelvic floor as a whole) responds to the fight or flight response of your autonomic nervous system, leading to chronic holding of your muscles, thus causing spasm and pain.
Sexual/physical trauma: past or recent sexual and physical trauma can cause unconscious tightening of the pelvic floor muscles.
Chronic inflammation: conditions such as chronic constipation, IBS, Crohn's disease, chronic UTI or yeast infections can eventually irritate the surrounding tissue, which can trickle down to the levator ani muscles.
Pudendal Neuralgia
Pudendal Neuralgia is a long-term pelvic pain syndrome that originates from damage or irritation of the pudendal nerve, the main nerve of the pelvis.
The pudendal nerve supplies areas of the pelvic floor such as:
Lower buttocks;
Perineum (the area between the rectum and genitals);
Area round the anus and rectum;
Scrotum and penis.
When the pudendal nerve is damaged, the pain feels like a burning, crushing, shooting, or prickling sensation. It may develop gradually or suddenly. It will also be worse when sitting down and improve with laying down or standing.
Pudendal neuralgia can happen if the pudendal nerve is damaged, irritated, or trapped.
Possible causes include:
Compression of the pudendal nerve by nearby muscles or tissue- – sometimes called pudendal nerve entrapment or Alcock canal syndrome;
prolonged sitting, cycling, horse riding or constipation (usually for months or years) – this can cause repeated minor damage to the pelvic area;
surgery to the pelvic area;
a broken bone in the pelvis;
damage to the pudendal nerve during childbirth – this may improve after a few months;
a non-cancerous or cancerous growth pressing on the pudendal nerve.
Constipation
Constipation occurs when a person does not regularly pass stool. This may also occur due to inadequate fiber intake, low physical activity, medications (eg: opioid use, blood pressure medications, antidepressants), irritable bowel syndrome, and changes in routine (eg: travel). Those who suffer from constipation usually produce dry, hard stools resembling rabbit pellets. Sometimes there may be pain and cramping in the abdomen, bloating, nausea, and loss of appetite.
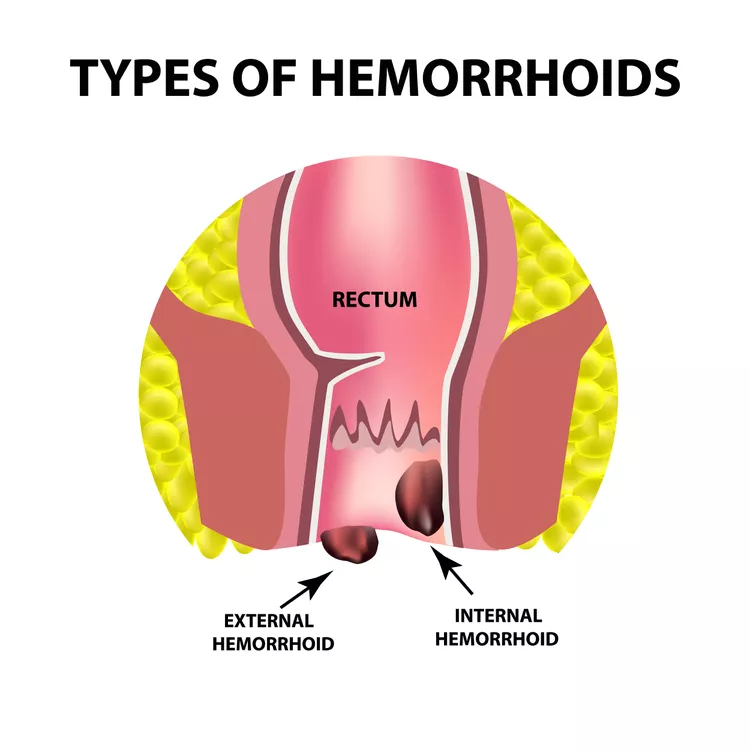
Hemorrhoids
Hemorrhoids are swollen blood vessels in the walls of your rectum or anus. Hemorrhoids are quite common in the smaller, milder form. They can become painful and itch and can leave blood on the tissue when you wipe.
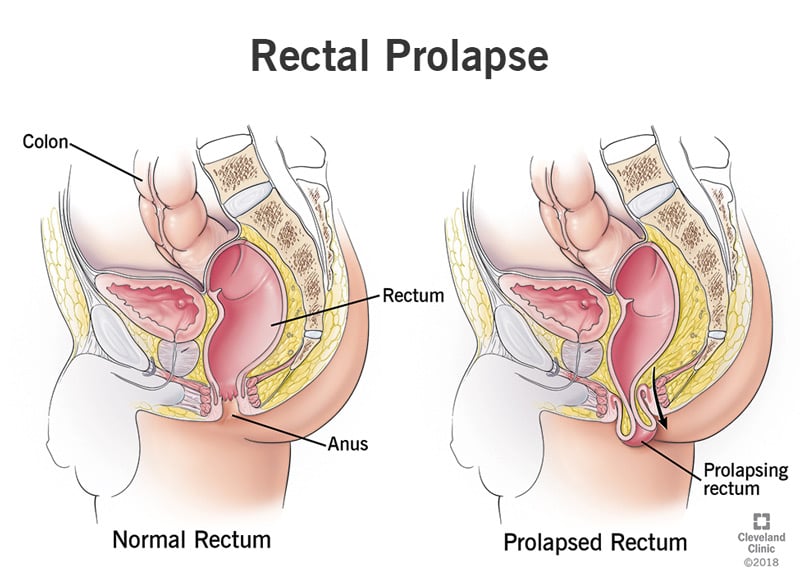
Rectal Prolapse
The rectum is the last part of your large intestine, and the anus is the opening through which feces exits your body. A rectal prolapse may be caused by weakening of your internal and external anal sphincters that hold your anus in place. They may feel or look like hemorrhoids, but unlike hemorrhoids, it doesn’t go away on its own. It MAY require surgical intervention, but conservative treatment is recommended before surgery is considered.
The reasons that rectal prolapse may occur may be due to:
Poor intra-abdominal pressure in sitting, standing, running, or any lifting/carrying;
Straining on the toilet while defecating;
Sudden movements (ie: tripping, falling down the stairs);
Sneezing.
Rectal prolapse can range from mild to severe. There are four types of rectal prolapse. The type can be identified by the movement of the rectum:
Internal prolapse (Grade I): the rectum starts to drop but has not yet pushed through the anus;
Partial prolapse (Grade II or III): only part of the rectum has moved through the anus;
Complete prolapse (Grade V): the entire rectum extends through the anus.
The symptoms of rectal prolapse tend to come on slowly. The first symptoms you’ll notice is the feeling that there is a bulge at your anus. With a mirror, you may be able to see a pink and/or red colored bulge peeking through your anus.
Additional symptoms may include:
Part of the rectum may protrude during bowel movements and may easily be pushed back in place;
Physical activity, such as walking, sitting, and exercising, may cause part of the rectum to push through the anus;
May be bleeding from the inner lining of the rectum;
Eventually, you may have trouble controlling liquid or solid bowel movements and gas from your rectum.
All the conditions above can be treated through a variety of treatments at Pelvic Health Center such as:
Myofascial release/massage to the affected muscles and entrapments;
Nerve glides;
Improving intra-abdominal pressure via upper/lower body strengthening, posture retraining;
Improving toileting mechanics;
Relaxing nervous system via vagus nerve stimulation;
Stretching affected muscles and soft tissues;
Visceral mobilizations to affected areas;
Shock wave therapy to affected areas;
Biofeedback to rectal muscles.
If you’re experiencing pelvic floor dysfunctions associated with the issues above, including rectal prolapse, pudendal neuralgia, constipation, hemorrhoids, and levator ani syndrome, please reach out to us at Pelvic Health Center in Madison, NJ to set up an evaluation and treatment! Feel free to call us at 908-443-9880 or email us at receptionmadison@pelvichealthnj.com
Works Cited:
https://my.clevelandclinic.org/health/diseases/14615-rectal-prolapse
https://www.healthline.com/health/levator-ani-syndrome#symptoms
https://www.carygastro.com/blog/levator-ani-syndrome-pelvic-floor-pain-and-how-it-is-treated
Read More:
Fascial Counterstrain of the Musculoskeletal System By Shannon Strauch, PTA, STMT-1 on 10/21/2024 How treating cartilage and fascia can help reduce joint pain and improve organ function The Impact of Long-Distance Cycling on the Pelvic Floor: Pudendal Nerve and Pelvic Dysfunction By Dr. Christine Martirez PT, DPT on 10/18/2024 Learn how long distance cycling can impact the pelvic floor
Are you ready to live pain free?
Request An Appointment